Abstract
To perform patient plan quality assurance (QA) on a newly installed MR-linac (MRL) it is necessary to have an MR-compatible QA device. An MR compatible device (MR-Delta4) has been developed together with Scandidos AB (Uppsala, Sweden).
The basic characteristics of the detector response, such as short-term reproducibility, dose linearity, field size dependency, dose rate dependency, dose-per-pulse dependency and angular dependency, were investigated for the clinical Delta4-PT as well as for the MR compatible version. All tests were performed with both devices on a conventional linac and the MR compatible device was tested on the MRL as well.
No statistically significant differences were found in the short-term reproducibility (<0.1%), dose linearity (⩽0.5%), field size dependency (<2.0% for field sizes larger than 5 × 5 cm2), dose rate dependency (<1.0%) or angular dependency for any phantom/linac combination. The dose-per-pulse dependency (<0.8%) was found to be significantly different between the two devices. This difference can be explained by the fact that the diodes in the clinical Delta4-PT were irradiated with a much larger dose than the MR-Delta4-PT ones. The absolute difference between the devices (<0.5%) was found to be small, so no clinical impact is expected.
For both devices, the results were consistent with the characteristics of the Delta4-PT device reported in the literature (Bedford et al 2009 Phys. Med. Biol. 54 N167–76; Sadagopan et al 2009 J. Appl. Clin. Med. Phys. 10 2928).
We found that the characteristics of the MR compatible Delta4 phantom were found to be comparable to the clinically used one. Also, the found characteristics do not differ from the previously reported characteristics of the commercially available non-MR compatible Delta4-PT phantom. Therefore, the MR compatible Delta4 prototype was found to be safe and effective for use in the 1.5 tesla magnetic field of the Elekta MR-linac
Export citation and abstract BibTeX RIS
1. Introduction
At UMC Utrecht, an MRI-linac (MRL) has been installed, combining magnetic resonance imaging (MRI) with a linear accelerator (linac). This MRL is an improved version of the one described by Raaymakers et al (2012). The MRL is equipped with a 7 MV flattening-filter-free (FFF) linac (Elekta AB, Stockholm Sweden) and a 1.5 tesla MRI-scanner (Philips Medical Systems, Best, The Netherlands).
By combining an MRI scanner and a linac, it is possible to simultaneously irradiate and create a high-quality image of soft-tissue contrast in the target area (Lagendijk et al 2014).
Before starting patient treatment, extensive quality assurance (QA) of the treatment plans needs to be performed to make sure the planned dose distributions are deliverable with the required accuracy. At our institute, QA of the pre-treatment plans is also performed for the MRL, although this plan will be adapted to the position and anatomy of the patient at the time of treatment. The post-treatment QA of the delivered plan is also performed at our institute. To perform such verification measurements, nowadays several commercial QA systems are available (Hussein et al 2013). However, at the moment of writing, the only commercial MR-compatible device available is the ArcCHECK-MR (Model 1220-MR, Sun Nuclear Corporation, Melbourne, USA). The performance of this device in the MRL has been evaluated by Houweling et al (2016).
In our department, a Delta4-PT phantom (Scandidos AB, Uppsala Sweden) (clinical Delta4) is used for the QA of the treatment plans. The performance of this device has previously been investigated by Bedford et al (2009) and Sadagopan et al (2009).
Together with the research and development department of Scandidos AB (Uppsala, Sweden) a prototype MR compatible Delta4 phantom (MR-Delta4) was developed. This MR-Delta4 is based on the commercially available Delta4-PT. The effect of these changes on the characteristics of the phantom is expected to be small and unclear. Furthermore, the basic design characteristics, like the small air volumes around the diodes, might influence the measurements due to the electron return effect (ERE) as well (Raaijmakers et al 2007, Reynolds et al 2014).
The purpose of this study is to characterize the MR-Delta4 phantom and compare these results to the characteristics of the clinical Delta4.
Therefore, the short-term reproducibility, dose linearity, field size dependency, dose rate dependency and dose-per-pulse dependency of both phantoms were evaluated.
All of these tests were performed on a conventional linac with an unflattened beam (FFF) for both the clinical Delta4 and the MR-Delta4. To study the effect of the presence of a 1.5 T magnetic field, all of the tests were repeated with the MR-Delta4 in the MRL.
2. Material and methods
2.1. Linacs
The conventional linac (Precise Treatment System, Elekta, Stockholm, Sweden) is equipped with a 6 MV FFF photon beam. The source-axis distance (SAD) of this linac is 100 cm, with a multi-leaf collimator (MLC) and 40 leaf pairs of 1 cm leaf width at the SAD. The dose maximum for this beam is a depth of 16 mm and the TPR 20/10 is 0.695.
The MRL is a combination of a modified 7 MV FFF (Elekta, Crawley, UK) accelerator and a modified 1.5 T MR system (Philips Ingenia, Best, The Netherlands). The SAD of the MRL is 143.5 cm, and it is equipped with 80 leaf pairs of 0.72 cm width at the SAD. The dose maximum of this beam is a depth of 13 mm, where the TPR 20/10 is 0.702.
Both accelerators were calibrated to deliver 1 Gy per 100 MU at the dose maximum, according to the NCS-18 Code of Practice (Nederlandse Commissie voor Stralingsdosimetrie (Stralingsdosimetrie, January 2008).
2.1.1. Phantoms
The Delta4-PT phantom is a cylindrical polymethylmethaacrylate (PMMA) phantom containing two orthogonal detector boards with 1069 p-type Si-diodes in total (Scandidos). To be used in the MRL, the device had to be made MR-compatible. Therefore, the feet of the device were taken off, adaptations were made to the network sockets and the power supply cables were extended to position the power supply outside of the 5 gauss line of the magnetic field area. In figure 1(A) the device is set up in the MRL.
Figure 1. The MR-Delta4 phantom in a regular QA setup (A) and the standard setup for performing all characterization measurements (B).
Download figure:
Standard image High-resolution imageThe phantom consists of two crossing arrays which are fixed in a cylindrical geometry. No differences between the arrays are expected. For the purpose of this study, the main detector board of the Delta4-PT phantom was taken out of the cylindrical phantom and embedded in a rectangular calibration phantom (Scandidos AB, Uppsala, Sweden) made of PMMA (figure 1(B). This allowed the insertion of an ionization chamber (IC) (Farmer NE 2571A IC, Qados, Sandhurst, United Kingdom), in a parallel orientation to the magnetic field (figure 1(B)) in the phantom at the same time for each measurement.
The standard measurement setup in the conventional linac was a source-skin distance (SSD) of 95.0 cm, resulting in a source-detector depth (SDD) of 99.75 cm (4.75 cm geometrical depth in PMMA, which is equal to 5.06 cm water equivalent depth). The standard setup at the MRL was an SSD of 137.3 cm, with an SDD of 142.0 cm.
All measurements were performed with the clinical Delta4 and MR-Delta4 in a conventional linac, and with the MR-Delta4 in the MRL.
2.2. Methods
No differences in performance between the different detectors are expected. Therefore, only the central diodes on the mainboard were investigated. For each test the three central diodes of the detector board were measured along with a simultaneous IC measurement (figure 1(B)). For each measurement the three diodes were averaged and then the average diode reading was divided by (i.e. normalized to) the corresponding averaged IC reading to eliminate possible linac output fluctuations. Deviations were calculated from the readings under reference conditions.
The reference field size used was 10 × 10 cm2, the dose rate was set to the maximum available, and 100 monitor units per measurement were given. The standard Farmer chamber, field size, dose rate and number of monitor units were applied unless otherwise noted.
2.3. Short-term reproducibility
The short-term reproducibility was examined by performing ten consecutive measurements for each linac-phantom combination. The reading of the three central diodes was normalized to the average reading of the ten IC measurements. The standard deviation and maximum deviation of the readings were calculated.
2.4. Dose linearity
The dose linearity was investigated by measuring the reading for 2, 5, 10, 20, 50, 100, 200, 500, 1000 and 3000 MU. All measurements were normalized to the 100 MU measurement. The standard deviation and maximum deviation of the readings were calculated.
2.5. Field size dependency
To investigate the field size dependency, 100 MU was delivered per measurement for field sizes of 2 × 2 cm2, 5 × 5 cm2, 10 × 10 cm2, 20 × 20 cm2 and 22 × 22 cm2. All measurements were normalized to the 10 × 10 cm2 field measurement.
For field sizes equal to and smaller than 5 × 5 cm2, a small volume ionization chamber (IC-04, IBA Dosimetry GmbH, Schwarzenbruck, Germany) was used instead of the Farmer chamber.
2.6. Dose rate dependency
The dose rate dependency was assessed by varying the pulse-rate frequency (PRF) in the linac.
The investigated dose rate range depended on the type of linac and modality of the photon beam.
For the FFF photon beam in the conventional linac 456, 229, 113, 57 and 25 MU min−1 were applied. In the MRL, dose rates of 680, 396, 366, 345, 341, 287, 171, 85 and 43 MU min−1 were used.
All measurements were normalized to the intermediate dose rate measurement (e.g. 113 and 171 MU min−1).
2.7. Dose-per-pulse dependency
The dose-per-pulse dependency was evaluated by changing the source detector distance (SDD) per measurement. In the conventional linac, SDDs of 80, 90, 100, 110, 120, 140, 142.7 and 150 cm were applied. All measurements were normalized to the measurement for an SDD of 100 cm.
By design, the tabletop of the MRL is not able to move in height and the SDD cannot be changed; therefore, this test was not performed in the MRL.
2.8. Angular dependency
Each system was irradiated with the conventional linac from a range of gantry angles to assess the angular dependency of the detectors. Particular attention was given around gantry angles of 90 and 270°, where the change in angular sensitivity was expected to be greatest. Measurements were also performed with the MRI-linac at angular increments of 30° (gantry angles were limited at the time of the measurement). All measurements were normalized to the reading of the gantry angle 0°.
2.9. Statistical analysis
For the short-term reproducibility and the dose rate dependency, because the samples were completely independent, the differences between the devices and linacs were tested for significance using the Kruskal–Wallis test. For all other experiments, where independency was not assured, a Friedman test was performed (IBM SPSS statistics, version 23).
3. Results
3.1. Short-term reproducibility
There was no significant difference (p = 0.266) in the short-term reproducibility for either the clinical Delta4 or the MR-Delta4 on both the conventional linac and the MRL (figure 2). The maximum deviation was 0.2%, which was observed for the MR-Delta4 phantom in the conventional linac.
Figure 2. The short-term reproducibility of the clinical and MR-Delta4 in a conventional linac and the MR-Delta4 in the MRL. Per phantom/linac combination, the reading is normalized to an average of ten measurements.
Download figure:
Standard image High-resolution image3.2. Dose linearity
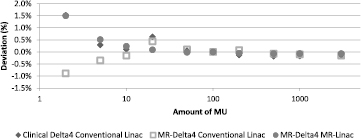
The largest deviations were observed for the 2 MU measurements for all phantom/linac combinations (figure 3). However, no significant difference (p = 0.717) was observed between the different devices.
Figure 3. The dose linearity of the clinical Delta4 and MR-Delta4 in a conventional linac and MRL. Per phantom/linac combination, the reading is normalized to the measurement of 100 MU; the X-axis is displayed on a log scale.
Download figure:
Standard image High-resolution image3.3. Field size dependency
An increasing deviation is observed when the field size decreases (figure 4). There was no significant difference observed (p = 0.196) between any of the phantom/linac combinations for the field size dependency.
Figure 4. The field size dependency of the clinical Delta4 and the MR-Delta4 in a conventional linac and MRL. Per phantom/linac combination, the reading is normalized to a 10 × 10 cm2 field size.
Download figure:
Standard image High-resolution image3.4. Dose rate dependency
There was no significant difference found (p = 0.478) between any of the phantom/linac combinations for the dose rate dependency, although there is an outlier for the MR-Delta4 in the MRL (36.5%) (figure 5). However, if this outlier is not taken into account, all other points are within 1% deviation.
Figure 5. The dose rate dependency of the clinical Delta4 and MR-Delta4 in a conventional linac and MRL. Per phantom/linac combination, the reading is normalized to an intermediate dose rate (around 120 MU min−1, depending on the linac).
Download figure:
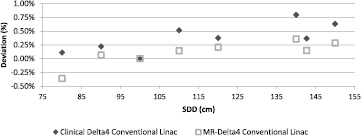
Standard image High-resolution image3.5. Dose-per-pulse dependency
The dose-per-pulse dependency, measured by increasing the SDD (80–140 cm), is presented in figure 6. All values were normalized to the reading at an SDD of 100 cm. All readings were within a 0.8% difference. There is a significant difference found (p = 0.008) between the samples in the clinical Delta4 and the MR-Delta4. The largest difference between two measuring points (at the same SDD) is 0.5% for an SDD of 80 cm. On all dose-per-pulse variations the clinical Delta4 shows a larger deviation than the MR-Delta4 phantom.
Figure 6. The dose-per-pulse dependency of the clinical Delta4 and the MR-Delta4 on a conventional linac. Per phantom/linac combination, the reading is normalized to the measurement at an SDD of 100 cm.
Download figure:
Standard image High-resolution image3.6. Angular dependency
The angular dependency, measured by varying the gantry angle, is presented in figure 7. All values were normalized to the reading at a gantry angle of 0°. There was no significant difference found (p = 0.174) between any of the phantom/linac combinations for angular dependency. The largest difference between two measuring points (at the same gantry angle) is 11.8% for a gantry angle of 270°.
Figure 7. The angular dependency of the clinical Delta4 and the MR-Delta4 in a conventional linac and MRL. Per phantom/linac combination, the reading is normalized to the measurement at a gantry angle of 0°.
Download figure:
Standard image High-resolution image4. Discussion
The characteristics of an MR-compatible Delta4-PT phantom were investigated in a transverse 1.5 T magnetic field in the MRL. These were compared with the results of the same tests performed on a conventional linear accelerator. Moreover, the results were compared to the clinical version of the Delta4-PT. No significant differences between any of the phantom/linac combinations were found for short-term reproducibility, dose linearity, field size dependency or dose rate dependency.
Feygelman et al (2009) and Sadagopan et al (2009) showed that the short-term reproducibility of the detector response was 0.1%, which is consistent with our measurements.
For dose linearity Bedford et al (2009) reported a Delta4 response for 5 MU that was better than 0.5%. Sadagopan et al (2009) showed a response within 0.25% for doses of 43 cGy (≈50 MU) and higher.
In this study, the results for ⩾5 MU are consistent with Bedford et al (2009) and Sadagopan et al (2009).
The largest deviation in dose linearity was +1.5% for the MR-Delta4 at the MRL. However, this deviation was found for measurements of 2 MU.
As seen in standard clinical practice, the lower the number of MU, the larger the deviation will be. For all readings at 2 MU the deviation is no larger than ±2%, which is the clinically accepted tolerance for this small amount. Therefore, this deviation is not clinically significant.
For the dose rate dependency Feygelman et al (2009) showed a variation in Delta4 response of no more than 0.8%. In this work, a difference of 36% was observed at PRF-values of 130 Hz (320 MU min−1) for the MR-Delta4 in the MRL. Excluding this point, the response variation for dose rate dependency was consistent with the literature (<1%).
The outlier in the dose rate dependency for the MR-Delta4 device in the MRL can be explained by the fact that these measurements were performed without a trigger signal, whereas all the measurements in the conventional linac were performed with the device connected to the triggering-signal of the linac. By design, there is no point on the MRL where a trigger cable can be connected since the gantry can rotate continuously. When there is no trigger cable connected to the device, the device switches to the so-called search mode and waits until it detects radiation on the detectors. The sampling window of this search mode is set at 300 Hz ± 10 Hz, which results in a sampling time of 3 ms. The PRF to get a dose rate of 320 MU min−1 at the MRL is 130 Hz, which gives a period of 7.8 ms. Calculations of these period times show that every 1st, 4th, 7th, 8th and 10th radiation pulse is not detected by the phantom.
Since the sampling window for the dose is set at 300 Hz, the same amount of missed pulses can be expected with PRF values for 260 and 65 Hz (double or half of 130 Hz).
In a clinical linac, Delta4 measurements are made in a triggered mode, so for the outcome of the QA measurements of volumetric modulated arc therapy (VMAT) plans there is no error expected. When measuring in an MRL, the measurement has to be made in an untriggered way, but since the width of the detected peak is small, about 50 Hz corresponds to an actual dose rate difference in the machine of 20 MU min−1. Furthermore, no effect on the VMAT plans is expected.
Feygelman et al (2009) showed a variation in the dose-per-pulse dependency of less than 0.4%. They varied the SDD from 102.7 cm to 68.8 cm. A comparison of these results in the same range of SDD shows a similar variation for all phantom/linac combinations. For the larger SDD Sadagopan et al (2009) found a variation of 0.25%, with a standard deviation of 0.6%. The measurements in this study fit within this range.
There was a significant difference observed for the dose-per-pulse dependency between the clinical Delta 4-PT and the MR-compatible version. However, the maximum absolute difference between the two phantoms is less than 0.5%. This statistically significant difference between the two devices can be explained by historical irradiation. The clinical Delta4 has been used in our institute for six years. This may have caused a decrease in sensitivity for these detectors. The absolute reading for all MR-Delta4 measurements, when no correction factors are applied, is on average 3% higher than for the clinical Delta4 device. If absolute calibration factors are applied, this difference will be removed.
In the detector boards, small air volumes around the diodes up to a few mm in size are evident in the CT scan. It is expected that the Lorentz force, acting on electrons within the air cavities, will change the diode readings, depending on the precise shape and size of the air cavities (Raaijmakers et al 2007). Also, the incident direction of radiation with respect to the magnetic field may cause a relative response difference (Raaijmakers et al 2007, Reynolds et al 2014). This is the likely explanation of the observed variation in angular sensitivity.
5. Conclusion
Short-term reproducibility, dose linearity, field size dependency, dose rate dependency dose-per-pulse dependency and angular dependency were investigated on a commercially available Delta4 phantom, as well as for the modified MR-compatible phantom. Both devices were tested in a non-MR environment (conventional linac) and the MR-compatible phantom was tested in an MR-environment (1.5 T MRL).
For the majority of tests, no significant differences were observed for either device in the conventional linac or MRL; however, for the dose-per-pulse dependency a significant difference was observed. This difference was within the clinical tolerance.
Therefore, it is concluded that the modifications applied to the original Delta4-PT phantom to make it MR-compatible did not result in any significant changes. The prototype system is suitable for safe and effective use in the 1.5 T magnetic field of the MRL.
Acknowledgments
We would like to thank Scandidos AB for their collaboration and providing us with an MR-compatible Delta4-PT phantom prototype, and in particular, Daniel Nystrom and Thomas Matzen of Scandidos AB for their contribution to this study.