Abstract
Wearable robotics, also called exoskeletons, have been engineered for human-centered assistance for decades. They provide assistive technologies for maintaining and improving patients' natural capabilities towards self-independence and also enable new therapy solutions for rehabilitation towards pervasive health. Upper limb exoskeletons can significantly enhance human manipulation with environments, which is crucial to patients' independence, self-esteem, and quality of life. For long-term use in both in-hospital and at-home settings, there are still needs for new technologies with high comfort, biocompatibility, and operability. The recent progress in soft robotics has initiated soft exoskeletons (also called exosuits), which are based on controllable and compliant materials and structures. Remarkable literature reviews have been performed for rigid exoskeletons ranging from robot design to different practical applications. Due to the emerging state, few have been focused on soft upper limb exoskeletons. This paper aims to provide a systematic review of the recent progress in wearable upper limb robotics including both rigid and soft exoskeletons with a focus on their designs and applications in various pervasive healthcare settings. The technical needs for wearable robots are carefully reviewed and the assistance and rehabilitation that can be enhanced by wearable robotics are particularly discussed. The knowledge from rigid wearable robots may provide practical experience and inspire new ideas for soft exoskeleton designs. We also discuss the challenges and opportunities of wearable assistive robotics for pervasive health.
Export citation and abstract BibTeX RIS

Original content from this work may be used under the terms of the Creative Commons Attribution 4.0 license. Any further distribution of this work must maintain attribution to the author(s) and the title of the work, journal citation and DOI.
1. Introduction
Neuromuscular disorders are diseases that pathologically originate in the musculoskeletal system, the nervous system, or the interfacing between the two, such as amyotrophic lateral sclerosis (ALS), muscular dystrophy, spinal cord injury (SCI), etc [1]. Strokes are now reclassified as a neurological disease according to the World Health Organization's new International Classification of Diseases (ICD-11) [2]. Although the clinical presentation of these diseases may vary, they normally affect muscle control and sensory feedback and result in symptoms such as muscle weakness or paralysis, muscle spasticity, and even non-functional muscular systems [1, 3]. Some neuromuscular disorders cannot be fully cured and thus rely on enhancing rehabilitation and quality of life [3, 4]. Although still growing, exoskeletons are promising assistive technologies for maintaining patients' activities of daily living (ADL) [5] as well as therapeutic devices for rehabilitation and treatment [6]. Thus, exoskeletons provide new and/or alternative solutions for both in-hospital and out-of-hospital healthcare towards pervasive health. By definition in the dictionary, pervasive refers to 'existing in or spreading through every part'. Pervasive health is defined as 'healthcare to anyone, anytime, and anywhere by removing locational, time, and other restraints while increasing both its coverage and quality' [7]. Although pervasive health sometimes has a broader definition including preventive proactive healthcare [7], our literature review is mainly focused on the studies within this direct definition—care anywhere beyond clinical settings for patients and their caregivers.
Neuromuscular disorders, cerebrovascular diseases, and other injuries and disabilities can lead to upper and/or low limb motor impairments and dysfunctions. Upper limbs are the key to human beings' manipulation with the environment and thus their motility is crucial to patients' independence, self-esteem, and quality of life. Upper limb exoskeletons have been developed and applied for assistance and rehabilitation in the past two decades [8] and have shown their feasibility and effectiveness [9, 10]. They have also been combined with other therapeutic solutions for neurological or neuromuscular treatment [10, 11]. However, not all robotic systems are initially designed with the full consideration of clinical use [12] and thus iterations are often required. Therefore, understanding both technical and patients' needs in both in-hospital and out-of-hospital settings is highly desired for wearable robot design.
Traditional exoskeletons for upper limbs are normally built upon rigid links and joints and apply forces and torques to upper limbs. Soft exoskeletons also called exosuits that are flexible, portable, and lightweight have also been successfully developed in recent years for various applications. Inspired by the controllable structures of textile materials, a variety of new textile actuators and softer and more compliant wearable robotics have been reported with remarkable studies ranging from material design, actuator design, to robotic design towards wearable textile robotics like everyday garments.
For wearable robotics, both rigid and soft, a number of literature review articles have summarized the recent research progress with different focuses, ranging from robotic designs to their applications. Gopura et al [13] and Muhammad et al [14] comprehensively reviewed upper limb exoskeleton system designs and Rasedul et al [15] compared the research prototypes and commercial types of upper limbs. Some articles specifically performed literature reviews for key components for wearable upper limb robotics including mechanical designs [16], control strategies [17], actuation systems [18], and motion planning [19]. Most of these articles are for rigid exoskeletons. In recent years, soft and textile exoskeletons are emerging. Due to the softness and compliance of such robots' materials, various studies have been performed with special focuses on smart materials and structures for motion generation. To this degree, some remarkable literature review articles have been performed for summarizing new materials, structures, actuators, and designs of soft and compliant structures and robotics [20–23]. Only one has reviewed both rigid and soft exoskeletons with a focus on the shoulder joint [5].
Wearable upper limb robotics by nature provide additional human mobility, which has broad applications. For pervasive healthcare, the applications of wearable robotics mainly include ADL assistance and patients' rehabilitation in various settings. Some specific domains have been studied in both research and clinical field. Mekki et al [10] reviewed robotic rehabilitation for SCI including both upper and lower limb robotics. Zuccon et al [24] and Xu et al [25] performed surveys about robotic rehabilitation after strokes. Gassert and Dietz [26] focused on studies using robotic devices for the recovery of sensorimotor function. Some other articles reviewed general rehabilitation robotics from different angles and with different scopes [27–34]. Although wearable upper limb exoskeletons have been used for both daily assistance and rehabilitation in clinical studies, there are still gaps between wearable robot design and patients' needs. For long-term use in both in-hospital and at-home settings, new technologies are highly desired with the consideration of comfort, biocompatibility, and operability. The recent progress in soft exoskeletons may provide new opportunities for pervasive health.
This paper aims to provide a systematic literature review of wearable upper limb exoskeletons for pervasive health considering both technical design perspectives and healthcare applications. The recent progress in both rigid exoskeletons and emerging soft wearable robotics and their applications in pervasive health is summarized. Particularly, this article covers the robot designs with the consideration of typical disease treatments, rehabilitation therapies, and assistance, aiming to provide integrated technical and clinical guidance. Upper limb exoskeletons provide not only effective therapies but also a promising solution for improving patients' self-esteem and quality of life. However, there are still technical challenges, and research contributions are highly expected towards affordable, ubiquitous, and comfortable assistance and treatment.
The rest of the paper is organized as follows: section 2 summarizes the upper limb kinematics and biomechanics. Section 3 classifies exoskeletons and gives an overall introduction. Sections 4 and 5 cover the technical designs of rigid and soft exoskeletons, respectively. Section 6 summarizes the research progress of wearable robotics as therapeutic devices for practical pervasive health applications. Section 7 discusses the challenges and opportunities, and section 8 concludes the paper.
2. Upper limb kinematics and biomechanics
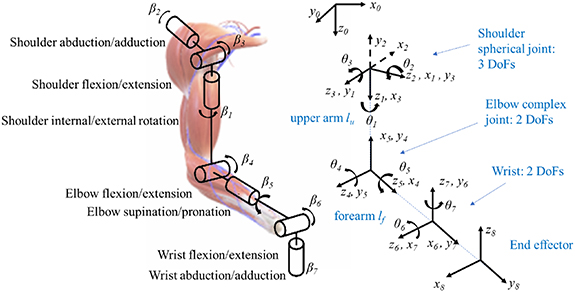
Exoskeleton designs require careful consideration of human biomechanics and kinematics. The upper limb motion involves the interaction of the nervous systems, musculoskeletal systems, and their interfaces. In human anatomy, the muscles that move the upper arm are those connecting to the humerus, which include the pectoralis major, latissimus dorsi, deltoid, and rotator cuff muscles. And the forearm movement is based on the triceps brachii, biceps brachii, brachialis, and brachioradialis. The overall upper limb movement can be considered as a kinematic chain consisting of three joints, the shoulder joint, elbow joint, wrist, and two links, the upper arm and forearm as shown in figure 1. The mobility can be simplified to seven degrees-of-freedom (DOFs). The shoulder joint has three DOFs, the shoulder internal/external rotation (β1), shoulder abduction/adduction (β2), and shoulder flexion/extension (β3); the elbow joint allows a two-DOF motion, elbow flexion/extension (β4) and elbow supination/pronation (β5). The wrist joint allows two-DOF wrist flexion/extension (β6) and wrist abduction/adduction deviation (β7) motion, which are associated with hand motion and will not be discussed in detail in this paper. This kinematic model is the basis for upper limb exoskeleton design as well as for rehabilitation estimation. The actual human joint mobility given by bones coupled with muscles usually involves a limited translation and cannot achieve a fully rotational motion. Using Denavit–Hartenberg (D–H) convention in figure 1, we briefly list the physiological range of motion (ROM) of each angle and the four corresponding D–H parameters in table 1. Robotic ROMs are often used as evaluation metrics for rehabilitation robotic design. A number of great reviews have been performed for hand rehabilitation [35, 36], which will not be the main focus of this paper.
Figure 1. Human upper limb kinematics model and its D–H convention.
Download figure:
Standard image High-resolution imageTable 1. Human upper limb ROM and D–H parameters [37].
| Joint | Physiological ROM of 
| i |

|

|

|

|
|---|---|---|---|---|---|---|
| Base | Zero |

| 0 |

|

| 0 |
| Shoulder | Internal rotation (−90°), external rotation (+90°) |

| −90° | 0 | 0 |
 +90° +90° |
| Shoulder | Abduction (−180°), adduction (+50°) |

| +90° | 0 | 0 |
 +90° +90° |
| Shoulder | Flexion (−180°), extension (+80°) |

| 0 |

| 0 |
 +90° +90° |
| Elbow | Extension (−10°), flexion (+145°) |

| +90° | 0 | 0 |
 +90° +90° |
| Elbow | Pronation (−90°), supination (+90°) |

| +90° | 0 |

|
 +90° +90° |
| Wrist | Flexion (−90°), extension (+70°) |

| +90° | 0 | 0 |
 +90° +90° |
| Wrist | Abduction (−15°), adduction (+40°) |

| 0 |

| 0 |

|
Although the above-mentioned seven DOF kinematic model has been widely used for understanding and analyzing human upper limb motion, the physical joint designs can be various for different DOF generations in both rigid and soft exoskeletons. In traditional rigid exoskeletons, the DOFs can be generated by actuators with rigid mechanical support or housing systems. In soft exoskeleton designs, more ideas have been proposed including those inspired by the human musculoskeletal system itself. For example, the shoulder, elbow, and wrist joint were modeled as a spheroid joint, a hinge joint, and an oval joint, respectively in [38]. More detailed analyses of human upper limb anatomy can be referred to [5, 39].
3. Classification of wearable robotics in pervasive health
Among rehabilitation and ADL assistive robots, there are two major types of robot designs, end effector based systems and wearable exoskeletons. End effector type robots are more like independent robotic manipulators and apply forces and torques to the human distal end and measure at the interface [40]; whereas exoskeletons are wearable and operated in parallel with upper limbs with multiple points connected. End effector types of rehabilitation robotics can provide motion trajectory of hand for therapy and estimation and are relatively easy to be customized to individual tasks; however, the human joint angles (βi ) during tasks cannot be directly not known from the robotic device [41]. Wearable exoskeletons are attached to and move with human arms and joints and provide forces and enhance mobility as a human-in-the-loop system. They can control human joints and provide multi-DOFs but are normally more complex to design and control [32]. Exoskeleton designs are more wearable, portable, and lightweight in recent years, enabling more application scenarios towards pervasive health.
Exoskeletons can be active (i.e. powered) or passive. With the first powered exoskeleton developed in the 1960s [42], there have been a great number of exoskeletons developed for ADL assistance, therapy and rehabilitation, to capability augmentation. Most of the powered exoskeletons are controlled by human physical or physiological conditions detected by sensors. These control inputs include force and torque, position and velocity, joint angle, electromyography (EMG), electroencephalogram (EEG), impedance, or hybrid. Different sensors and signal processing and data fusion methods have been developed to estimate human inputs and conditions for robotic control. As human interfaces, surface EMG (sEMG) measures electrical signals on the skin that are generated in the underneath muscle during its contraction and relaxation, which is generally believed to be able to represent neuromuscular activities including motor intention [43–45]. In addition, sEMG has also been studied to estimate torque and impedance for robotic control [46]. EEG detects electrical activities on the human scalp and is widely used as a noninvasive brain interface. EEG coupled with EMG has also been attempted for motor intention estimation for robotic control [47, 48]. Passive exoskeletons have no actuation systems and are often used for ergonomic support to prevent injuries, reduce workload, and augment human capabilities, which have been used in different industrial sectors. Some passive exoskeletons are available in the market for occupational health and safety [49, 50]. Designed with the consideration of human biomechanics, it is believed that these industrial use passive exoskeletons can prevent work-related musculoskeletal disorders for occupants [51]. This literature review article will not cover preventive health cases. Occupational exoskeletons have been explicitly reviewed by [51–53].
Exoskeletons can be rigid or soft. Most of the exoskeletons used for pervasive health applications are still rigid. In the recent decade, soft exoskeletons, also called exosuits, have been emerging with the fast growth of soft robotics technology. The term 'soft robotics' includes two types of designs, compliant joints or actuators within rigid robots and continuum robotics [54]. Continuum robots consist of actuatable structures with constitutive materials (rigid or soft) able to achieve controllable curves. Actually, as a broad concept, soft robots are not always completely soft and sometimes contain rigid structures. Similarly, exosuits are not fully soft and sometimes use rigid cables and support structures. The power and batteries are also rigid and often hidden in the backpack. Sometimes the term 'exosuit' can be broader and refer to all types of wearable robots that are like 'suits' even with rigid parts in the design. Thus, the boundary between rigid and soft exoskeletons is actually vague. In this article, we will use the following definition to classify rigid and soft exoskeletons: rigid-joint exoskeletons, simplified as rigid exoskeletons sometimes, refer to those that use motors, linear actuators, traditional pneumatic/hydraulic actuators, and other rigid actuators at human joints to generate human motions and DOFs and thus the main robot body is rigid as a whole; whereas soft exoskeletons (i.e. exosuits) refer to those that use flexible materials and/or structures for motion and DOF generation although such flexible structures can include small rigid parts and cables and the overall wearable robot body is soft and/or flexible like a garment.
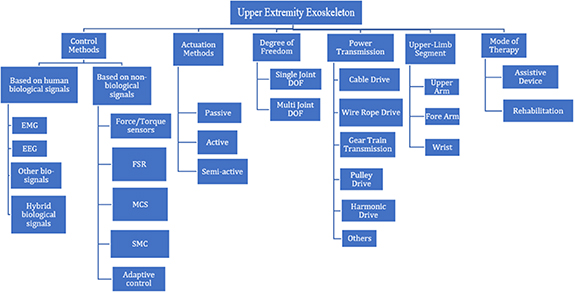
For a fully autonomous exoskeleton with human interaction, no matter rigid or soft, the overall robot design needs to consider all the key components in a systematic way as shown in figure 2. To this end, exoskeletons can also be classified according to their control methods, mechanical designs (i.e. actuation and power transmission methods), as well as target pervasive health applications. Although human inputs have been explored for active soft exoskeletons, most of the existing studies of advanced controls are mainly focused on rigid-joint exoskeletons due to the emerging state of the soft exoskeletons. The typical mechanical designs are also mainly for rigid-joint exoskeletons. Thus, we will start with traditional rigid-joint exoskeletons and illustrate the key components for exoskeleton designs in section 4 followed by soft exoskeletons in section 5. The knowledge from traditional rigid designs may provide practical experience and inspire new ideas for soft exoskeleton designs.
Figure 2. Categorization of upper limb exoskeletons.
Download figure:
Standard image High-resolution image4. Rigid-joint exoskeletons
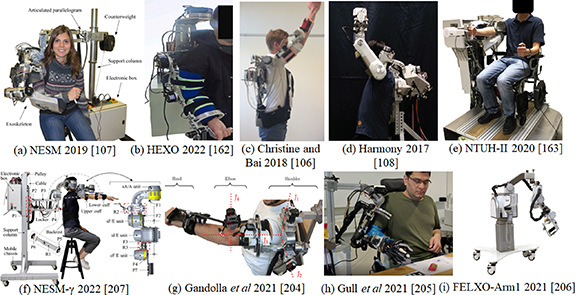
Given target application scenarios, the physical design of upper-limb exoskeletons needs to consider DOF, sensing and control methods, actuators, power transmission, and the upper-limb segment to be controlled according to the needs and specifications. For example, exoskeletons for back support in work conditions emphasize reducing the applied loads and/or muscle activities [55] whereas rehabilitation robots are designed to achieve targeted rehabilitation tasks such as planned motion trajectory and joint movement. To this end, the hardware design and the control methods vary. Also when targeting assisting different joint motions, the physical design can be different as well. In this section, we technically review the key components for rigid-joint upper limb exoskeletons. Notably, Muhammad et al [14], Maciejasz et al [28], Gopura et al [13], and Xu et al [25] comprehensively listed typical exoskeleton designs including both hardware and control; in this section, we will not list designs and will focus on the necessary techniques for designing key components of exoskeletons. Although such key techniques are mainly used for rigid-joint exoskeletons, the knowledge may inspire new soft designs as well. Figure 3 shows typical rigid-joint exoskeletons in recent five years.
Figure 3. Recent rigid-joint exoskeleton design examples.
Download figure:
Standard image High-resolution imageThe rehabilitation robots should be capable of providing the patients with repetitive and task-oriented treatment. To this end, the controller design should be adaptable considering to patient's personalization and rehabilitation stages. Considering patients' conditions, the control strategies for such robots can be categorized into (1) patient-passive and (2) patient-cooperative control strategies [6] depending on the patient's muscle control conditions. Patient-passive controlled exoskeletons can assist patients to achieve predefined trajectories with zero required efforts and thus are suitable for those without any muscle control. A number of control strategies ranging from proportional–integral–derivative (PID) controller [56] to more advanced methods have been considered for this type [17, 57]. Patient-cooperative control strategies consider patients' motion intention and should enhance human-robot interaction towards better treatment thus motion intention estimation is significant in rehabilitation exoskeleton design. Feedback control with motion intention estimation thus has been broadly studied [58]. Considering technical designs, upper limb exoskeletons need to consider human input signals, controller design, actuation, and power transmission. According to the patient's condition and the associated rehabilitation tasks, the overall design can be varied. Different human sensing and inputs have been studied to estimate human motion intention to enhance human-exoskeleton interaction.
4.1. Human inputs
4.1.1. EMG
EMG is the record of the electrical activities of muscles and motor neurons. Electrical activation potentials of skeletal muscles can be measured through EMG signals, showing spikes in signals when the muscle cells are electrically stimulated and no signals when these muscles are at rest. EMG-based continuous motion prediction methods can be generally categorized into two types, (1) model-based approaches that use muscle, kinematic or dynamic models to estimate certain motion parameters and (2) model-free approaches that are mainly data-driven [59]. sEMG is the detection of signals from the skin surface and is predominately utilized for non-medical applications in contrast to intramuscular EMG. sEMG has been widely used as the input for exoskeleton control or human-robot interaction. EMG electrode placement also needs to be well considered to optimize signal acquisition for targeted motions [60].
When using sEMG as real-time control inputs, there are generally three steps: (1) data segment for real-time analysis; (2) signal pre-processing for generating EMG features including both time-domain and frequency-domain features; and (3) linear regression and/or classification with results inputting to or combined with the controller. Figure 4 shows the overall architecture of using EMG-based model-free methods for upper limb exoskeleton control. Most real-time control systems implement linear classifiers. Some classification methods like neural network, motion direction estimation, common spatial pattern, minimum distance classifier, support vector machines, blind source separation, linear discriminant analysis (LDA), random forest, and neuro-fuzzy, dynamic recurrent neural network are common classifiers applied in EMGs and EEGs.
Figure 4. Typical architecture of EMG-based upper limb exoskeleton control using model-free methods.
Download figure:
Standard image High-resolution imageEMG intensity is directly related to the muscle force [61] and thus has been used to estimate joint angles [62–65], torques [66–71], forces [72] in exoskeleton control and actuation as well as for impedance control [73]. Classification-based control methods can be single or multifunctional and there is a performance trade-off. For classification, the training datasets need to be carefully collected and also sufficient to predict desired motion classes or parameters. A number of studies directly feed EMG features into classification or regression algorithms to train the desired output. Liu et al [74] developed a myoelectric control method for rehabilitation robots using linear/nonlinear regression trained with EMG and position. Lei [75] extracted time, frequency, and time–frequency domain features of EMG to train a backpropagation neural network. In [73], EMG was used as the control input for a hybrid impedance-admittance control method for an exoskeleton. In [76], an upper extremity motion pattern recognition using a modified multi-channel EMG feature was proposed, in which time and frequency domain features were used. A modified rank of the short-time Fourier transform feature was implemented through modification of the conventional features. Loconsole et al [77] proposed a torque control of the shoulder and elbow joints through online prediction using sEMG based method with feedforward time delay neural networks. Forces exerted in the sagittal plane when the length of the muscle remained relatively constant under tension were recorded using the sEMG signals. In [78], an algorithm based on LDA and backpropagation was developed for training multilayer perceptron neural networks for pattern recognition and feature extraction of EMG signals. In some studies, physical models are also considered in the data-driven method. Kiguchi and Quan [79] developed an effective EMG-based controller for a four-DOF upper limb exoskeleton using a muscle-model adjusted weight matrix fed into a neuro-fuzzy modifier.
For EMG-based rehabilitation exoskeletons, a great number of remarkable designs have been proposed and developed in the past two decades. Some of them have also been used and studied in clinical trials as discussed in section 5. In these therapies, exoskeletons need to support patients' rehabilitation tasks and/or patient-exoskeleton cooperation and be programmable and adaptive to patients' personalization and rehabilitation stages and EMG can help facilitate the interaction. In addition, EMG signals are also useful for fatigue monitoring but can be limited to some individuals or become extremely weak after suffering a stroke. In addition to rehabilitation therapies, some exoskeletons have shown positive effects on affecting human mental state by improving quality of life and ADL. Some exoskeletons assist patients by providing mobility to the target limb, which is more lightweight and portable. In [80], a low-cost real-time embedded EMG-driven RobHand was developed, which provides an active-assistive technology to improve the range of arm motion, strength, motor function of the upper limbs and provide improved ADL. More examples of ADL are discussed in section 5.3.
4.1.2. EEG
EEG measures the electrical activities along the scalp, which is believed to represent brain activities and is often used as a primary tool for brain-computer interfaces (BCIs). A robot is commonly interfaced with EEG signals for human intention estimation. BCIs are often used to control the robot to achieve the desired motion by selecting prior constructed motion patterns such as reaching targets [81, 82], and upper limb motions [83–86]. Low-frequency portion in EEG signals contains the important feature of the motion. For controlling exoskeletons, EEG signals are normally processed for upper limb motion estimation using classification or pattern recognition algorithms. Al-Quraishi et al [87] reviewed EEG-based control for both upper and lower limb exoskeletons and prosthesis. EEG-based exoskeletons are actually not as extensively studied as EMG-based designs. In [88], an exoskeleton named MAHI Exo-II was developed using EEG to estimate the intentions of a stroke survivor while identifying movement-related cortical potentials. Xiao et al [89] adopted an Emotiv EEG headset to control a four-DOF exoskeleton for sequential upper limb imagined motions. In rehabilitation robots and therapies, EEG is sometimes used as a diagnostic and/or tool in addition to control inputs for exoskeletons. In these cases, the rehabilitation robots may be passive [90].
Although EEG has been used for robotic arm control, EEG-controlled exoskeletons overall are still in an emerging stage due to the complicated neural states and the corresponding signal processing, pattern recognition, and classification. Although muscle atrophy and absence of EMG signals are notable possibilities with patients, EMG signals are specifically applicable in areas with a high signal-to-noise ratio (SNR), fatigue monitoring, and less to no training required. Consequently, EEG signals are preferred for patients with the absence of EMG signals. In rehabilitation therapies, EEG-based motor imagery may provide opportunities for enhancing neuroplasticity and synchronized monitoring and analytics. In addition, EEG, as one of the primary BCIs, is still believed to be promising in predicting motion intention for robotic devices.
4.1.3. Hybrid biological signals
The hybrid inputs can be achieved through a sequential or simultaneous fusion of two human biological signals, mostly EMG-EEG, to provide a more comprehensive human interface for robot control. Lalitharatn et al [91] conducted a literature review on the hybrid fusion of EMG-EEG-based control approaches that can be used in bio-robotics, in which design methods were discussed, buttressing the main features with advantages of this approach. Although EMG-EEG has been studied as a promising human interface for manipulators and end effector type robotic devices [92], it has not been widely attempted yet for wearable upper limb exoskeletons. Kawase et al [93] developed a real-time controlled exoskeleton for paresis using hybrid EMG-EEG with EMG being used to estimate joint angles. In [94], a regularized cost function of artificial neuron network is presented as an estimation method for instinctual control of an upper limb exoskeleton with EMG and EEG signals tested in an arm simulator, the model predicted grab motion from EMG signals and arm movement motions from EEG signals.
EMG-EEG hybrid inputs provide unique features for exoskeleton control including those from both muscle and brain activities. Such inputs can not only provide motor estimation and intention prediction but also be used as an evaluation tool for rehabilitation therapies. However, synchronized EMG and EEG detection requires relatively more complicated sensing system design and control strategies.
4.1.4. Other bio-signals
In addition to EMG and EEG, some other biological signals also show the potential as human inputs for robotic device control. Among them, sonomyography (SMG) is the detection of change in muscle thickness or deformation using ultrasound imaging, depicted by temporal and spatial features. SMG has been studied to estimate and predict human motion intention and motion pattern recognition recently [95, 96]. Engdahl et al [97] classified user performance during clinical tests of upper limb transradial procedure, based on analogous SMG spatial features, while exploring the repeatability isolation of SMG control signal over a short period of time during pre-prosthetic training. An experimental comparison was also performed in [98] to evaluate the effect of SMG-based and sEMG-based human-machine interface (HMI) on finger motion classification for more precise control and manipulation. Mechanomyography (MMG) is a technique that involves recording and estimating the mechanical activities of active skeletal muscle fibers using specific acoustic systems. Due to its discriminative power, higher bandwidth, and SNR, it can be considered a control method for signal extraction. Castillo et al [99] designed an MMG armband, which enabled the control of normal force distribution applied in varied sections of an upper limb loss of a transracial patient.
The above-mentioned other biological signals have not been applied directly to the upper extremity exoskeleton but have been used in upper limb prosthesis control. However, the mode of signal extraction and control methods may be considered to be applied to exoskeleton design for upper limbs. In exoskeleton designs, EMG is still the most commonly used biological signal for providing human inputs in control methods.
4.1.5. Non-biological inputs
In many cases of rehabilitation exoskeletons, patients' joint angles and torques need to be measured for both human inputs for control and rehabilitation estimation. Thus, encoders for joint angle detection and/or torque sensors are also a typical hardware design with a number of notable studies using different control strategies. Crea et al [100] developed and clinically validated a powered exoskeleton with two control modes, position control and torque control for elbow spasticity treatment. Wu et al [101] developed a gravity-balanced exoskeleton for active rehabilitation training of the upper limb using both encoders and torque sensors.
Non-biological signal based control methods can also estimate the motion intention of users by analyzing the force and/or torque signals through a variety of sensors attached to the upper limb exoskeleton. Direct measurement of mechanical outcomes of muscles can be achieved by using force sensors, load sensors, strain gauges, or measuring intended limb joint torque and acceleration. Among them, the muscle circumference sensor (MCS) measures the circumference change caused by muscle, which can be used to estimate force and torque. Kim et al [102] developed an MCS to estimate the torque of the human elbow joint and then some studies started to leverage MCS in exoskeleton control. In [103], a model was developed for a reference-based adaptive control algorithm to drive the exoskeleton in the desired impedance fashion and the radial basis function neural network was employed to extract the desired motion intention (DMI). Khan et al [104] extracted the human DMI through a damped least square algorithm implementing a passive adaptive control algorithm as an estimation method. They also presented a MCS with load cells to estimate the DMI generated using passivity adaptive control [57].
Another notable non-biological sensor for feedback control is the force sensing resistor (FSR), which is a device able to measure changeable resistance with applied force and has been adopted for detecting forces exerted in human-exoskeleton interaction. In [105], a power-assist robot was proposed with an intentional reaching direction intention method using FSRs for real-time estimation of motion intention. Christensen and Bai [106] developed a shoulder exoskeleton using a double parallelogram linkage using FSR for interaction force measurement. Among all these non-biological signal based controls, sensors have been selected and utilized together with the control strategies.
4.2. Control
4.2.1. Impedance and admittance control
Impedance and admittance control are bio-inspired control methods considering the conversion between position and torque. The impedance controller aims to generate interaction force from position error, which is analogous to preventing disturbance to the task trajectory [56, 73]. Admittance control is the opposite and aims to allow motion from force/torque feedback and facilitate human-exoskeleton interaction. In rehabilitation exoskeleton designs, impedance and admittance controllers can be in the task space or the joint space. Task-space also called Cartesian-space impedance controllers are more preferred due to the fact that it is directly related to task trajectory design and task-space motions are three-dimensional compared to the n-dimensional joint space [6]. In this case, the sensor selection and placement need to align with the control strategy. Actually, in all design cases, the sensing, control, and other hardware design must be considered as a whole according to the required tasks. A number of recent studies implemented impedance controllers in their exoskeleton designs such as the NeuroExos Shoulder-elbow Module (NESM) [107], and the harmony exoskeleton [108]. Some researchers also designed impedance controllers with biological signals to enhance human inputs [109, 110] and with adaptive control to achieve adaptive impedance control [109, 111]. In [73], a hybrid impedance-admittance control was proposed using EMG inputs.
4.2.2. Sliding mode control (SMC)
To ensure quick dynamic response with insensitivity to time variations and reduced disturbance, SMC can be implemented to control the dynamics of a nonlinear system. A time delay estimation (TDE) based on the sliding mode and Jacobian transpose (JSTDE) controller for adaptive control of the ETS-MARSE upper limb exoskeleton was proposed in [112] to accommodate variations of unspecified nonlinear kinematic and dynamic in upper extremity exoskeleton. Brahmi et al [113] presented a second-order sliding mode compliant controller based on human inverse kinematics for active rehabilitation mode using TDE on an ETS-MARSE upper extremity exoskeleton robot. Instability within the system resulting from minor challenges due to external noise was attenuated through adaptive gains and TDE. Bembli et al [114] modeled and simulated a two-DOF upper limb exoskeleton design, implementing SMC and individual joint control of dynamical systems achieved through computer torque control (CTC) for precise linearized trajectory tracking. A simulated general assistive exoskeleton controller that does not require a sensor system for estimation of the user's motion intention but requires only the joint position information to function by conforming to the user's force was presented in [115]. Rahman et al [116] developed a seven-DOF upper extremity exoskeleton namely ETS-MARSE, which implemented SMC control to accommodate passive arm movement during rehabilitation sessions. Efficiency and feasibility of adaptive control based SMC with TDE that permits perturbed and uncertain nonlinear dynamics was proposed in [117]. SMC methods presented in [112–118] were known for their dynamic behaviors and negligence to external disturbances and have been applied to a robot-aided shoulder rehabilitation exoskeleton for tracking arm trajectories. A combination of a conventional PID controller and sliding mode controller to form a hybrid system was proposed in [119] also using the ETS-MARSE. The results showed that this control method achieved precise tracking performance and reduced external disturbance. A five-DOF upper-limb robot from [120] was improved in [121], in which a fuzzy sliding mode controller was proposed for precise position tracking and to be robust to model uncertainties while implementing an inverse dynamic method as the control input from the system.
4.2.3. Adaptive control
For dynamical models with varying parameters, adaptive control systems automatically compensate discrepancies in systems dynamics, unlike SMC control is time-dependent. SMC and adaptive control have also been integrated to achieve adaptive SMC. Kang and Wang [120] developed a system to enhance the safety of a five-DOF upper extremity exoskeleton, an adaptive controller design was proposed for precise tracking, improved fault tolerance and safety. Exoskeleton design optimization plays a key role in upper extremity exoskeletons, Nasiri et al [122] presented a new adaptive controller for assistant level optimization of exoskeletons, using a combination of adaptive feedforward and feedback controllers. Brahmi et al [123] developed an adaptive tracking control strategy that used backstepping approach coupled with time-delay estimation to estimate unknown dynamics and compensate for external bounded disturbances. Alshahrani et al [124] presented a four-DOF upper extremity exoskeleton utilizing ipsilateral-to-ipsilateral synchronous and ipsilateral-to-contralateral mirror control mechanism for volitional control of the upper limb exoskeleton. Table 2 summarizes the control methods based on non-human biological signals.
Table 2. Control methods based on non-human biological signals.
| References | Control method | Control mode | Support provided | Coordinate system evaluation | Sensor type |
|---|---|---|---|---|---|
| [119] | PID-sliding mode | Adaptive control | Modified DH parameters | ||
| [120] | Adaptive control | Adaptive control | DH parameters | ||
| [111] | MCS | Adaptive impedance control | Active | DH parameters | Force, load sensor |
| [112] | SMC, JSTDE | Adaptive control | Hall sensor, force sensor | ||
| [113] | SMC | Adaptive control | Active | Modified DH parameters | Hall sensor, force sensor |
| [114] | SMC, CTC | Adaptive control | Simulated | ||
| [105] | FSR | Admittance control | Active | Jacobian matrix | Force sensor |
| [115] | SMC | Simulated | Jacobian matrix | Force sensor | |
| [121] | FSMC | Simulated | DH parameters | ||
| [103] | MCS, load cells | Adaptive impedance control | Jacobian matrix | ||
| [116] | SMC | Adaptive control | Passive | Jacobian matrix | Force, torque |
| [117] | SMC | Adaptive control | Passive | ||
| [118] | SMC | Adaptive control | Passive | Jacobian matrix | |
| [57] | MCS | Adaptive control | Active/Passive | Jacobian matrix | Force, load |
4.3. Actuation and power transmission
4.3.1. Actuators
Robot and human joints are moved or rotated by the forces and/or torques generated through actuators that convert various sources of stored energy into mechanical work. To attain maximum torque to the upper extremity joints for exoskeletons, a variety of actuators have been developed and adopted in hardware design. Most of the rigid-joint exoskeletons use common actuators including motors, linear actuators, traditional pneumatic/hydraulic actuators, and other rigid actuators at human joints to generate human motions and DOFs, and thus the main robot body is rigid as a whole. Such active actuators create an ensuring operating condition through a varying ROM at changing speeds and torque. Some also combine different actuators in exoskeleton design for different motion generation. In [125], a pneumatic muscle actuator (PMA) was implemented on a four-DOF upper extremity exoskeleton prototype, in which the designed PMA achieved different proposed assistive exercises by controlling the movements of the shoulder and elbow joints. A rehabilitative elbow orthosis was designed in [126], using a flexible fluidic actuation system to control the elbow motion of the wearer while providing functional support. In [127], rotational hydroelastic actuators mounted on the joints of the user were validated [128], an upper limb exoskeleton. In [129], a combination of pneumatic artificial muscles and back-drivable motors constituted the development of a pneumatic-electric hybrid actuation system for an exoskeleton with one DOF at the elbow joint. Manna and Dubey [18] provide a detailed analysis of available actuation systems for the development of portable upper extremity exoskeletons, in which actuation mechanisms, types of actuators, mounting options, and considerable factors for selecting an actuation system were extensively explained.
4.3.2. Power transmission
Power transmission in exoskeletons should provide the necessary power, be kept simple, have low inertia, and usually depend heavily on the actuation method implemented. These features are required to convert a research prototype into a commercial product of an upper extremity [15]. The transmission of power from the actuators to the joints of the upper limbs can be achieved using gear drives, cable drives, linkages, harmonic drives, pulley drives and other types of drives. Actuators located at desired points for joint motion require less power transmission for a limited distance from the points of force application when applying a linkage mechanism type. Some power transmissions operate smoothly, less noisily with high precision, which is achieved by positioning the actuators away from the place of force effect while establishing a connection through the application of a cable-driven mechanism [5]. Gear-driven mechanisms may increase the overall weight of the exoskeleton with the challenging issue of back drivability when using this type of power transmission. However, problems of backlash can be solved using a harmonic drive for upper extremity exoskeletons. Generally speaking, the power transmission needs to be designed with actuation systems.
5. Soft exoskeletons
Exosuits are soft exoskeletons that are more portable, wearable, and biocompatible. Although soft actuators have been used in rigid-joint exoskeletons, they are normally used for connecting rigid links and designs. Exosuits are normally textile- or fabric-based, which has promised results for both enhancing performances and compensating for neuromuscular deficiencies. Most of the exosuits are composed of an actuation system and wearable components, and the absence of a rigid structure omits the issue of misalignment between the joints of users and the robot so the safety and kinematic transparency stand out among the many benefits of using exosuits [130]. As aforementioned, the exoskeleton's principal objective is passive rehabilitation. While performing these tasks, the exoskeleton user leaves his arm immobile, and the exoskeleton is in control of moving the arm articulations in accordance with a therapist-preprogrammed pattern [131]. The performance of these exosuits is evaluated by their weight and muscle need reduction. Figure 5 shows typical exosuits in recent years and table 3 summarizes the designs and applications.
Figure 5. The development of upper limb exosuits.
Download figure:
Standard image High-resolution imageTable 3. Summary of soft upper limb exosuit designs and applications.
| References | Supported movements | Control method | Actuation system | Application |
|---|---|---|---|---|
| Nycz et al [132] | Fingers and elbow flexion/extension | — | Bowden-cable and DC motors | Home-care physical therapy |
| Cappello et al [133] | Elbow flexion/extension | EMG | Bowden-cable and DC motors | ADLs assistance |
| Abe et al [134] | Elbow and wrist | EMG | Weaved Mckibben muscle (pneumatic) | — |
| O'Neill et al [135] | Shoulder flexion/extension | Manual control | Pneumatic | Rehabilitation |
| Proietti et al [136] | Shoulder elevation and elbow extension | Dynamic GC and JTT controllers | Pneumatic | Rehabilitation |
| Dinh et al [137] | Elbow flexion/extension | EMG | Bowden-cable and DC motors | Help patients affected by bilateral brachial plexus injury |
| Li et al [138] | Elbow flexion/extension and forearm pronation/supination | Imitate human motion | Flexible band and DC motors | Help stroke survivors |
| Lessard et al [139] | Humeral rotation in/out, elbow flexion/extension, wrist pronation/supination, lateral shoulder raise, and forward shoulder raise/lower | Passive | Tendon-based Bowden cable and DC motors | Help users with single-arm impairment |
| Chiaradia et al [130] | Elbow flexion/extension | EMG-based untethered control architecture | Bowden-cable and DC motors | ADLs assistance |
| Wei et al [140] | Elbow flexion/extension | Passive | Bowden-cable and DC motors | Assist hemiplegic patients |
| Kim et al [141] | Elbow and shoulder flexion/extension | PID Voice | Bowden-cable and DC motors | Lifting and holding heavy loads |
| Pont et al [131] | Elbow and shoulder flexion/extension | Super twisting SMC | Bowden-cable and DC motors | Rehabilitation therapies |
| Little et al [142] | Shoulder flexion/extension | PID admittance (Gravity compensation controller) IMU | Bowden-cable and DC motors | At-home rehabilitation |
| Seth et al [143] | Elbow flexion/extension | — | Nylon thread and DC motors | Help stroke survivors |
| Elor et al [144] | Elbow extension/flexion and shoulder abduction/adduction | VR Mirror Visual Feedback | Bowden-cable and DC motors | Immersive physio-rehab robotic-assisted games |
| Ismail et al [145] | Elbow flexion/extension and wrist pronation/supination | Proportional-Integral (PI) | Bowden-cable and DC motors | ADLs assistance |
| Samper-escudero et al [146] | Elbow and shoulder flexion/extension | sEMG for monitoring | Bowden steel cables and DC motors | Assist the upper limbs flexion |
| Hosseini et al [147] | Elbow flexion/extension | sEMG | String and DC motors | Single and dual-arm elbow assistive |
| Lotti et al [148, 149] | Elbow extension/flexion | EMG | Bowden-cable and DC motors | Assisting human movement in healthy and impaired individuals |
| Georgarakis et al [150] | Shoulder flexion/extension | DF, DFF, and IF | Bowden-cable and DC motors | ADLs assistance |
| Sy et al [151] | Elbow flexion/extension | EMG for monitoring | Hydraulic-based miniature fluid transmission tubes | Rehabilitation and ADLs assistance |
| Ismail et al [145] | Elbow and shoulder flexion/extension | SMC | Bowden-cable and DC motors | Rehabilitation |
| Park et al [152] | Arm flexion/extension | Temperature control | SMA fabric muscle | Rehabilitation |
5.1. Cable-based actuation system
Cable-based actuation systems are intrinsically soft and flexible and can be coupled into textile design easily. Such actuation methods have been the most widely used in soft exoskeleton design by far. The enhanced wearability and ergonomics of exosuits driven by Bowden cables allow users to move freely and place the actuation stages far from the end-effector (EE). Although this actuation stage has advantages in durability, lightweight, safety, and flexibility, controlling such exosuits has some intrinsic limitations [137]. The friction and backlash between the Bowden sheath and the cable decrease the system performance and complicate system control [153–155].
Nycz et al [132] developed a soft exosuit based on fabric structures using DC motors and cables for flexion and extension of fingers and elbows. This type of exoskeleton enables the targeted end-users to wear the glove during the assembly to ensure precise component placement. This lightweight, soft cable-actuated glove and sleeve allow patients to rehabilitate in their homes with more accessibility to care and more cost-efficient therapy. Cappello et al [133] developed a similar design for elbow joints to actuate both the flexion and the extension with a single motor, which enables the actuation stage to be more compact and energy efficient. In order to conserve power during static configuration, a clutching mechanism is also included in the design, preventing the motor from holding the joint position for an extended period of time. Dinh et al [137] proposed a soft exoskeleton composed of stretchable fabric made of a mixture of elastane and polyamide to conform to the morphology of the wearer while enhancing ergonomics, durability, and flexibility. It is also composed of non-stretchable fabric made of nylon webbing to resist fabric deformation caused by cable tensions. Li et al [38, 138] proposed a primary prototype of bio-inspired wearable soft upper-limb exoskeleton for stroke survivors. Their goal was to construct an exosuit that is light and flexible that can reach similarity with the human body. Lessard et al [139] developed Compliant Robotic Upper-extremity eXosuits (CRUX) to help users with single-arm impairment. They use passive control that synchronizes one arm's position with the other arm's measurement position. CRUX encompasses flexible and compliant augmentation for the upper extremity, enabling users to do activities like bilateral mimicry. Chiaradia et al [130] developed a tethered fabric-based exosuit for the elbow joint. They presented an untethered control architecture to compensate for gravity and detect motion intention. Wei et al [140] proposed an exosuit based on human biomechanics for rehabilitation training of hemiplegic patients. For this purpose, the structure of the exosuit has to be optimized so as to minimize man-machine interaction force, which this force causes arm discomfort. It was claimed that the proposed exosuit reduces the man-machine interaction force by 10%–15%. Pont et al [131] proposed an exosuit called ExoFlex which was designed to aid in the rehabilitation of the shoulder and elbow. ExoFlex is constructed from a basis of fabric to which certain small, stiff pieces of nylon that were 3D printed at specific spots are connected to route the transmission Bowden cables in conjunction with metallic sheaths. A position super-twisting SMC has been designed and implemented, demonstrating the adaptation capability of ExoFlex to different wearers' arms and its stability in the presence of the user's torque. Samper-Escudero et al [146] designed a textile-based exosuit combined with different layers of fabrics using a force-compliant sewing pattern. This design helps disperse forces throughout the arm's large and stiff surface, which resolves the textile friction and slipping issues.
In exosuit designs, human inputs are also considered for control. Hosseini et al [147] developed a novel sEMG-driven soft exosuit using the twisted string actuators for the purpose of compensating the user's muscular activity while adding and removing loads in both single and dual-arm tasks. Lotti et al [148] developed an HMI-based exosuit that worked in tandem with biological muscle contraction. They developed a high-level controller using EMG signals and kinematic data to estimate the joint torque and a low-level controller that provided the required assistance. Little et al [142] increased the adaptability of their exosuit by incorporating shoulder elevation angle into their previous gravity compensation (GC) controller, so as to adapt the controller to the user's shoulder configuration. In this investigation, the inertial measurement unit (IMU) calibration procedure is needed, which is time-consuming, and their future objective aims at removing the calibration phase and fixing the sensors to the exosuit. Seth et al [143] designed a smart exosuit that can link to the user's smartphone and collect any necessary medical data. To overcome the drawbacks of the Bowden cable, they used nylon thread to reduce the load on the motors and also prevent the whirling of the cable while it is being extended.
5.2. Pneumatic and hydraulic actuators
Pneumatic actuators and artificial muscles and their control methods have been widely studied and integrated into rigid exoskeletons [150, 156]. They have been applied in rehabilitation robotic device designs as well [157] but most of them are used to connect rigid support systems. Recently, a few fully soft exosuits have been reported using pneumatic actuators for motion generation. O'Neill et al [135] developed a fully soft exosuit with textile-based inflatable actuators anchored to the torso and aimed at improving severe stroke rehabilitation by reducing therapist fatigue as shown in figure 5(j). Abe et al [134] weaved thin McKibben muscles to fabricate new artificial muscles and the results show that more displacement was able to be achieved compared to a single artificial muscle. Proietti et al [136] developed a multi-joint soft exosuit for upper limb assistance and rehabilitation using dynamic GC and joint trajectory tracking controllers. IMU sensors were used to control the pressure for the pneumatic actuators.
Using hydraulic actuators, Sy et al [151] developed an exosuit based on hydraulic-driven soft artificial muscles. The experimental results showed that the relationship between the input displacement of the syringe plunger and the muscle elongation is linear, which simplifies the kinematic model and controlling approach. They developed a kinematic model to determine the elbow angle from muscle length. It has been experimentally demonstrated that the lightweight exosuit can lessen the workload placed on the user's muscles.
5.3. Shape memory materials
Although a variety of textile-based actuators have been developed in the research stage such as nanowires, few have been practically used in upper limb soft exoskeleton design. Among them, actuators based on shape memory materials have been attempted by researchers. Park et al [152] developed a shape-conformable exosuit using SMA spring-based fabric muscles. They proposed a forced air-cooling fan-integrated fabric muscle to increase the cooling rate of the SMA spring, which increases the actuation speed. This work was able to provide a stable cyclic actuation within a defined temperature range while increasing the repeated actuating speed. SMA-based actuators have been used in soft robotic designs; however, few have been physically implemented for exoskeleton design yet.
6. Wearable robotics in pervasive health
Neuromuscular disorders, cerebrovascular diseases, injuries, and other disabilities can cause motor function deficits with different onsets including hemiparesis, bradykinesia, paralysis, etc. Some progressive neuromuscular disorders such as Parkinson's disease, ALS, pathologically originate in the nervous system or neuromuscular junctions and thus the desired assistance and/or therapies vary. Due to the patients' conditions and the corresponding training modules, there are four major types according to [6]: (1) patient passive robot active, (2) patient-robot cooperative, (3) patient active robot passive, and (4) robot resistive. Powered exoskeletons are active robotics and thus the second type of patient-robot cooperation is the most considered case using rehabilitation robots. This section aims to discuss the expected treatment outcomes, the desired training tasks, and the corresponding exoskeleton designs considering specific treatment of diseases.
6.1. Stroke rehabilitation
Stroke is among the top three most common causes of death and a primary cause of disabilities in most countries [158]. Clinical studies have shown strong evidence that exercise has positive physical and psychosocial effects on patients after strokes [159]. The main goal of robot-assisted stroke rehabilitation is to effectively leverage the residual motor capabilities of patients and utilize the brain's neuroplasticity to perform the exercise and motor relearning. Such rehabilitation exoskeletons need to be able to adapt to patients' needed tasks and recovery stages. Stroke rehabilitation has five stages—hyperacute (first 24 h), acuate (first 1–7 d), early subacute (7 d to 3 months), late subacute (3–6 months), and chronic phase (after 6 months) according to the stroke recovery and rehabilitation roundtable taskforce [160]. The first three months after stroke is the most rapid recovery period during which the brain has high neuroplasticity and spontaneous recovery typically occurs. In this stage, intensive therapies are performed both in medical settings and at home. Patients will reach a plateau in their rehabilitation recovery most certainly by 6 months. In addition, hemiparesis is also a common after-effect of stroke and the restoration of normal motor function in the hemiplegic upper limb is less than 15% among individuals [161]. Maintaining ADL is also necessary to improve patient's quality of life after strokes.
Both EE type robotic devices and exoskeletons have been used in randomized controlled trials (RCT) for subacute and chronic stroke rehabilitation. Examples of commercialized rehabilitation exoskeletons include the Armeo Spring, Armeo Power, and Myomo and those of research ones include Harmony [108], NESM [107], HEXO [162], NTUH-II [163], Aalborg University Exoskeleton [106], ALEx [164], EXO-UL8 [165], FELXO-Arm1 [166], CleverARM [167], etc, with typical ones shown in figure 2. In addition, concomitant therapies have also been adopted to enhance rehabilitation including virtual reality [168] and conventional stroke therapies. In these therapies, patient-exoskeleton cooperative tasks are often pre-programmed, and the subjects are required to accomplish the tasks to achieve the endpoint trajectories.
To evaluate the rehabilitation outcome, the testing group with exoskeleton-assisted therapies is often compared with that with conventional therapies. To assess the effectiveness, the ROM in upper limb neurorehabilitation therapy offers a comprehensive assessment together with meta-analysis that can measure motor control (e.g. Fugl-Meyer Assessment of the arm, a.k.a. FMA arm), muscle strength and tone, upper limb capacity, and basic ADL [177]. Veerbeek et al [177] performed a review and concluded that robot-assisted upper limb rehabilitation improves synergy-independent motor control of the shoulder/elbow and wrist/hand, but the overall effects are limited compared to the control group normally with conventional therapies. Lee et al [174] compared EE and exoskeleton robots for chronic stroke rehabilitation and found that no intervention-related adverse event was identified, and EE showed a better performance. O'Neill et al [135] evaluated an inflatable exosuit on a clinical population to reduce therapist fatigue. Table 4 shows typical RCT studies and/or clinical applications using exoskeletons. Previous studies showed that robot-assisted training has positive effects on motor impairment treatment and spasticity but inconsistent effects on functional capacity and ADL [178, 179].
Table 4. Studies of exoskeleton-assisted therapies for upper limb rehabilitation.
| Device name | Year | Stroke stage | Tasks | Intensity | Result |
|---|---|---|---|---|---|
| ARM-Guid [169] | 2006 | Chronic | Reaching | 45 mins, 24 sessions over 8 weeks | No difference compared to the control group |
| T-WRE [170] | 2009 | Chronic | Playing computer games | 30 mins, five times per week for 8–9 weeks | T-WREX can lead to modest gains, but no different from the control group |
| EMG-controlled wrist robot [171] | 2013 | Chronic | Repetitive wrist tracking | 20 sessions, 3–5 sessions per week within 5–7 weeks | Significant improvements in muscle strength and clinical scales |
| BCI-Exo complex [172] | 2017 | Subacute Chronic | 3 mental tasks | Ten BCI training sessions each lasting up to 40 min | Recovery in the BCI was observed in both subacute and chronic subgroups of patients |
| HAL-SJ [173] | 2019 | Acute | ADL | Combination with occupational therapy less than 3 h per day | Combination with occupational therapy affects ADL function |
| Armeo Powe [174] | 2020 | Chronic | Goal-directed reaching | 30 mins, 5 d a week for 4 weeks | EE is better than exoskeletons |
| Armule [175] | 2021 | Subacute | Desired trajectories in the game | 45 mins daily, 5 d per week, for 4 weeks | Can improve upper limb motor impairment, ADL, and kinematics after stroke |
| L-EXOS and VR [176] | 2022 | Chronic | Reaching and composing a virtual puzzle | 45 mins, three sessions per week over a period of 6 weeks | A much higher improvement of the robotic group was observed |
Although not all RCTs show more effective performance than conventional therapies for acute and chronic stroke rehabilitation, robot-assisted rehabilitation therapies have irreplaceable advantages: (1) Rehabilitation exoskeletons with programmable tasks can increase the efficiency of therapies especially in treating larger group of patients [32], which not only ensure patients' accessibility to rehabilitation therapies but also assist therapists. (2) Due to the capability of pre-programmed trajectories, exoskeletons can provide desired tasks with controllable applied force to ensure accurate therapies as needed. (3) Human interfaces are normally adopted within exoskeleton designs as discussed in section 4, which are also tools for quantitively accessing patients' performance in the rehabilitation progress. In addition, these tools such as BCIs can also indicate neural activities and more concomitant therapies may be enabled. Thus, research efforts are highly desired to improve exoskeleton design considering clinical needs and requirements as well as to provide more clinical evidence of the effectiveness of using such robotics in rehabilitation. The monitoring capability may also provide a new path to reveal physiological mechanisms that are not fully understood yet.
6.2. SCI
SCI is one of the most devastating injuries causing disabilities with about 60% of cervical SCIs resulting in tetraplegia [180]. According to the American Spinal Injury Association (ASIA), the severity of SCIs can be classified into five levels (ASIA-A to ASIA-E) by considering the motor and sensory function impairments [181]. Although the mechanisms of spinal plasticity are not fully clear [182], SCI rehabilitation also leverages central nervous system plasticity to achieve functional improvements [183]. Among them, restoring arm and hand functions is a top priority for patients with tetraplegia [184]. A few studies indicate that intensive robot-assisted therapies that have been used for stroke rehabilitation can be effective for SCI patients with residual motor capability as well [185]. However, it is still unclear what type of robot-aided intervention contributes to motor recovery for SCI patients [186].
Exoskeletons specifically designed for incomplete SCI rehabilitation are still emerging and clinical trials are not as many as for stroke rehabilitation. Fitle et al [187] designed the Mahi Exo II Rehabilitation Exoskeleton which was tested on subjects with incomplete SCI. Results showed that only less impaired upper limbs have enough control to perform movements without extreme inflection points. Pehlivan et al [188] developed the RiceWrist-S to assist in the rehabilitation of forearm muscles for patients with incomplete SCI. This exoskeleton has three rotational DOFs in the wrist and forearm and can provide an improvement in subjects' grip strength. Yozbatiran and Francisco [189] reviewed robot-assisted therapies for upper limn after cervical SCI and comprehensively listed the recent clinical studies for SCI patients. They concluded that randomized clinical trials are still needed to optimize protocols for SCI rehabilitation and function improvement. In addition, concomitant therapies such as neuromuscular electrical stimulation are also attempted with robotic therapies to restore upper limb functions [190].
6.3. Neuromuscular disorders and ADL
A number of robotic devices that were proposed primarily for use in motor rehabilitation of stroke patients have later been introduced to other neurologic disease treatments, such as multiple sclerosis [191, 192], cerebral palsy [193, 194], and Parkinson's disease [195], but most of them are EE based. The use of an exoskeleton in these neuromuscular diseases is emerging in recent years and the corresponding RCT studies are very limited. Lugo-Villeda et al [196] developed an exoskeleton for children with neuromuscular disorders that aims to reproduce the movements performed by a physical therapist. Raciti et al [197] conducted an RCT to investigate the use of exoskeletons for improving upper limb bradykinesia in Parkinson's disease and the results showed a greater improvement in the primary outcome measure. There is a high potential for using exoskeletons to improve the rehabilitation of patients with sensorimotor impairments.
People with motor impairments usually have difficulty performing everyday tasks like eating and drinking. Even after rehabilitation therapies as discussed above, full motor recovery is limited among patients. Thus, improving ADL is significant to enhance patients' independence and quality of life as well as reduce caregivers' loads. Different from rehabilitation exoskeletons, those for ADL need to have the following characteristics: (1) lightweight and portable so that daily activities can be achieved without bulky equipment in everyday settings; (2) human intention understanding to enhance assistance; (3) highly adaptive and autonomous without well-designed tasks and trajectories; (4) affordable for more population.
Sui et al [198] designed a wearable exoskeleton for daily assistance that is lightweight and mobile. This type of design enables the user to move around rather than be limited to using the device in one specific area. An exoskeleton coupled with a Microsoft Kinect camera was proposed by Latt et al [199] to help users feed themselves without assistance from a caregiver. This design focuses on giving the user a sense of independence while also using their own limb to activate rehabilitation simultaneously. In order to accommodate patients that suffer from these complications, Li et al [38] developed a bio-inspired soft exoskeleton, in which the artificial muscles were modeled after human muscles to create the most natural motion. In recent years, more compliant soft exosuits have been explored and developed as summarized in section 5, which shows high potential to achieve ubiquitous assistance in the near future.
7. Challenges and opportunities in pervasive health
According to the Centers for Disease Control and Prevention stroke fact [200], there is a new stroke patient every 40 s. Other neuromuscular disorders affect 14 million people globally [200]. The high expenditure of in-hospital healthcare for chronic conditions calls for new technologies for pervasive health for both patients and their families and caregivers. Wearable robotics provide a powerful and promising solution for pervasive health including both rehabilitation and ADL assistance in different settings. Remarkable studies have been done in the past half-century since the first active exoskeleton was developed in the 1960s. Although emerging, soft exoskeletons have shown big advantages and high potential to provide assistance and healthcare in everyday life. Notable products have been available in the market, however, most of the current exosuits are passive and designed for back support and injury prevention in short- or long-term use. There are still challenges as well as opportunities for exoskeletons to enable pervasive health.
7.1. Mechanical design and adaptability
In practical conditions, patients' physical conditions including their weights, sizes, physical conditions, needed rehabilitation and assistance can vary significantly. Even for one patient's treatment, the needed rehabilitation and/or assistance tasks as well as human inputs can differ as well. For physical exoskeleton design, one of the main challenges is the misalignment of rotating axes between human and exoskeleton models causing kinematic incompatibility [201]. Such misalignment causes uncomfortable wearability, inaccurate control, and even safety issues for wearers [202]. Although strategies have been proposed, highly adaptive exoskeletons with perfect physical connections still do not exist [201]. Soft exoskeletons provide adjustable structures that can be adaptive to patients with different weights and sizes; the control strategies with the change of tasks remain a difficult issue for soft robots, especially with more than two DOFs. Actually, soft exoskeletons with higher DOFs and adequate human control are still rare. The knowledge from rigid wearable robots may provide practical experience and inspire new ideas for soft exoskeleton designs.
7.2. Difficulty in ADL assistance for patients
Although there is still a need to improve exoskeleton design considering clinical needs and requirements, rehabilitation robots have been explicitly studied in clinical trials. However, exoskeletons for ADL assistance are still in the research stage and there is a long way to go for such exoskeletons to become daily available products. ADLs include everyday living tasks and are much more complicated than a few repeatable motions for joint exercises. For example, moving an arm to achieve basic drinking and eating needs seven DOFs [205], which none of the current soft exoskeletons can do. Actually, limited active exosuits have been designed for ADL assistance because task and trajectory based control is needed for such tasks. Nonetheless, soft bodies are way more complicated to control not to mention the various soft structures and designs with textiles in soft exoskeletons. Thus, there are still opportunities and needs for developing new technologies for patients' everyday assistance.
7.3. Affordability
In pervasive health, the high medical expenditure on chronic conditions can cause financial burdens to those families and thus low-cost customized assistive technologies are highly desired. Although still rare, the authors foresee that open source hardware design will be a future direction of assistive technologies.
8. Conclusion
In this paper, we systematically reviewed the recent progress on wearable robotics for pervasive health with a focus on the design and development of both exoskeletons and soft exosuits. Clinical studies of using exoskeletons for different rehabilitation therapies and ADL are also summarized and discussed. For rehabilitation purposes, upper limb exoskeletons can contribute to human motor recovery by enhancing motor relearning by leveraging neuroplasticity. RCTs using exoskeletons for post-stroke rehabilitation therapies have been conducted and promising results have been shown. Although the rehabilitation of other common neuromuscular disorders and SCIs may also utilize human neuroplasticity, not many RCTs for exoskeleton-based rehabilitation are attempted, and clinical evidence is still lacking. Considering different purposes and domains, we discuss the challenges and opportunities of designing exoskeletons for practical applications in pervasive health. This article also hopes to inspire new ideas for wearable robot designs with new human interfaces and compliant materials with the consideration of clinical needs.
Acknowledgments
This study is funded by the National Science Foundation (Grant Nos. 2222110 and 2135620). We sincerely appreciate the support to enable this study.
Data availability statement
The data cannot be made publicly available upon publication because they are not available in a format that is sufficiently accessible or reusable by other researchers. The data that support the findings of this study are available upon reasonable request from the authors.