Abstract
A generic formalism is proposed for reference dosimetry in the presence of a magnetic field. Besides the regular correction factors from the conventional reference dosimetry formalisms, two factors are used to take into account magnetic field effects: (1) a dose conversion factor to correct for the change in local dose distribution and (2) a correction of the reading of the dosimeter used for the reference dosimetry measurements. The formalism was applied to the Elekta MRI-Linac, for which the 1.5 T magnetic field is orthogonal to the 7 MV photon beam. For this setup at reference conditions it was shown that the dose decreases with increasing magnetic field strength. The reduction in local dose for a 1.5 T transverse field, compared to no field is 0.51% ± 0.03% at the reference point of 10 cm depth. The effect of the magnetic field on the reading of the dosimeter was measured for two waterproof ionization chambers types (PTW 30013 and IBA FC65-G) before and after multiple ramp-up and ramp-downs of the magnetic field. The chambers were aligned perpendicular and parallel to the magnetic field. The corrections of the readings of the perpendicularly aligned chambers were 0.967 ± 0.002 and 0.957 ± 0.002 for respectively the PTW and IBA ionization chambers. In the parallel alignment the corrections were small; 0.997 ± 0.001 and 1.002 ± 0.003 for the PTW and IBA chamber respectively. The change in reading due to the magnetic field can be measured by individual departments. The proposed formalism can be used to determine the correction factors needed to establish the absorbed dose in a magnetic field. It requires Monte Carlo simulations of the local dose and measurements of the response of the dosimeter. The formalism was successfully implemented for the MRI-Linac and is applicable for other field strengths and geometries.
Export citation and abstract BibTeX RIS

Original content from this work may be used under the terms of the Creative Commons Attribution 3.0 licence. Any further distribution of this work must maintain attribution to the author(s) and the title of the work, journal citation and DOI.
1. Introduction
The combination of a radiotherapy unit with a MRI scanner allows direct visualization of the target during the actual radiotherapy by providing excellent soft tissue contrast in real time. This will allow the development of high-precision MRI-guided radiotherapy. Several integrated MRI guided devices are under development or in clinical use (Fallone 2014, Keall et al 2014, Lagendijk et al 2014, Mutic and Dempsey 2014). Beside the technical differences between systems, such as the magnetic field strength, photon beam energy spectrum and the orientation of the magnetic field relative to the photon beam, all deliver the dose in the presence of a magnetic field.
As a magnetic field only affects charged particles, it does not affect photon trajectories, and therefore the photon fluence will not change in a magnetic field. The Kerma is not affected since, the energy transferred to the electrons is the same with or without a magnetic field. However, the magnetic field will change the trajectories of the resultant electrons via the Lorentz force, and will consequently affect the whole dose distribution in several way's. The impact of the magnetic field on the dose distribution depends on the magnetic field strength and its orientation relative to the photon beam, and also on the energy of the electrons. Examples of changes in the dose distribution are in the buildup region, the depth of the maximum dose, the penumbra regions, near density interfaces and also in regions of transient charged particle equilibrium (Raaijmakers et al 2007, 2008, Oborn et al 2009, 2010, Keyvanloo et al 2012).
For reference dosimetry in a magnetic field, the magnetic field effects have to be taken into account and standard protocols have to be adapted, in which reference dosimetry is the process of determining the absorbed dose to water at a point under reference conditions (Almond et al 1999, Andreo et al 2000, Aalbers et al 2008). There are two issues to be considered relative to a reference setup with a photon beam quality without a magnetic field. First is the change in local dose distribution due to the change in electron trajectories. Second, the magnetic field has an influence on the reading of the dosimeter used for reference dosimetry and this influence also has to be included in the adapted formalism (Smit et al 2013).
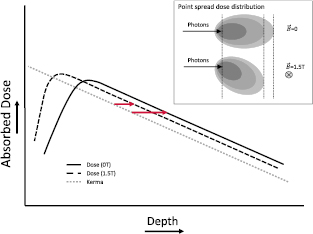
The dose distribution in an area of transient charged particle equilibrium (i.e. beyond dose maximum) changes due to the magnetic field, for example in the isocenter at 10 cm depth for a 10 × 10 cm2 field. At such a location, which is commonly chosen as the reference setup, the local dose distribution is different relative to the dose without a magnetic field due to the change in electron trajectories around the photon interaction point (Wolthaus et al 2016a). The electrons effectively deposit their energy in a different location. To clarify this effect, consider a broad photon beam with a magnetic field perpendicular to the central axis. In this case, the electrons trajectories will curve, which results effectively in increased energy deposition closer to the photon interaction point and reduction of the dose deposited downstream (figure 1). Thus at any specified depth (beyond the depth of the dose maximum) the absorbed dose will be lower with a magnetic field than without a magnetic field. The net effect will depend on the magnetic field strength and its orientation (Raaijmakers et al 2008).
Figure 1. A schematic depth dose curve with and without a magnetic field perpendicular to the photon beam and the Kerma in water which is independent of the magnetic field. The arrows indicate the difference in energy deposition relative to the Kerma. To illustrate the change in dose distribution around an interaction point, point spread dose distributions are shown.
Download figure:
Standard image High-resolution imageIdeally the change in detector reading due to the magnetic field would be proportional to the change in local dose. However, the response of some detectors, such as ionization chambers, may be influenced by the magnetic field. The change in reading depends on the dosimeter used and can be of the order of several percent for air-filled ionization chambers which are commonly used for reference dosimetry. It has been shown by several groups that the raw reading changes in a magnetic field, depending on the magnetic field strength, orientation of the magnetic field relative to the photon beam, chamber type and the orientation of the chamber (Meijsing et al 2009, Reynolds et al 2013, Smit et al 2013, O'Brien et al 2016, de Prez et al 2016b, Wolthaus et al 2016b, Spindeldreier et al 2017, Malkov and Rogers 2017a). The chamber reading depends on the average path length of the electrons inside the air-filled cavity, which will be affected by the presence of the magnetic field due to the Lorentz force (Meijsing et al 2009). The Lorentz force also affects the local electron fluence in the medium around the chamber, which in turn changes the local dose as described above as well as the inflow of the electrons into the cavity of the chamber. The variation of the electron influx will affect the reading of the ionization chamber (Meijsing et al 2009). Currently, no code of practice is yet available for performing reference dosimetry in the presence of a magnetic field and therefore existing protocols have to be adapted. A standard formalism, such as presented in the TRS-398 (Andreo et al 2000), TG-51 (Almond et al 1999) and NCS-18 (Aalbers et al 2008), was adapted by O'Brien et al (2016) according to the formalism presented by Alfonso et al (2008), which is a formalism for reference dosimetry of small and non-standard radiation fields. The adaptation of O'Brien et al includes a correction of the absorbed dose-to-water coefficient ( ) in the presence of a magnetic field which was determined by Monte Carlo calculations for several ionization chambers. To accommodate for the magnetic field Malkov and Rogers (2017a) used a different approach and adapted the standard formalism by introducing a single correction factor for all changes from the reference conditions. This factor combines the standard beam quality correction and the magnetic field corrections and was determined using Monte Carlo simulations of ionization chambers.
) in the presence of a magnetic field which was determined by Monte Carlo calculations for several ionization chambers. To accommodate for the magnetic field Malkov and Rogers (2017a) used a different approach and adapted the standard formalism by introducing a single correction factor for all changes from the reference conditions. This factor combines the standard beam quality correction and the magnetic field corrections and was determined using Monte Carlo simulations of ionization chambers.
The presented formalism in this paper introduces two correction factors to the existing reference dosimetry formalisms: a correction for the change in dose distribution due to the magnetic field and separately a correction for the change in reading of the ionization chamber. This approach makes a distinction between the different corrections to the dosimetry formalism needed to account for the effects of the magnetic field. Furthermore, the formalism presented here facilitates measurement of the change of reading due to the magnetic field by individual departments and comparison with Monte Carlo simulations of ionization chambers and calorimetry measurements. This approach was used for the clinical introduction of the MRI-Linac at the UMC Utrecht (Raaymakers et al 2017).
2. Formalism
In the existing codes of practice such as e.g. TRS-398 (Andreo et al 2000), TG-51 (Almond et al 1999) and NCS-18 (Aalbers et al 2008) the absorbed dose-to-water is given by

Where  is the machine specific beam quality,
is the machine specific beam quality,  the reference beam quality used for calibration of an ionization chamber,
the reference beam quality used for calibration of an ionization chamber,  is the absorbed dose-to-water at the reference point for beam quality
is the absorbed dose-to-water at the reference point for beam quality  ,
,  the absorbed dose-to-water calibration coefficient at the reference beam quality, and
the absorbed dose-to-water calibration coefficient at the reference beam quality, and  is the beam quality correction factor which corrects for the difference in dose-to-water calibration coefficient between the reference beam quality
is the beam quality correction factor which corrects for the difference in dose-to-water calibration coefficient between the reference beam quality  and the beam quality
and the beam quality  . The reading
. The reading  of the dosimeter corrected for pressure, recombination, polarity, relative humidity and temperature is given by
of the dosimeter corrected for pressure, recombination, polarity, relative humidity and temperature is given by

where  is the raw dosimeter reading,
is the raw dosimeter reading,  the factor to correct the response for temperature and pressure,
the factor to correct the response for temperature and pressure,  for relative humidity,
for relative humidity,  for polarity effect and
for polarity effect and  for incomplete charge collection due to recombination. The reading is corrected by equation (2) to meet the reference conditions.
for incomplete charge collection due to recombination. The reading is corrected by equation (2) to meet the reference conditions.
To determine the dose in presence of a magnetic field, the standard formalism (equation (1)) is adapted by including two factors. First a dose conversion factor to correct for the difference in local dose with and without a magnetic field is added, and secondly a correction to the reading of the detector obtained in the presence of the magnetic field is applied.
As explained in the introduction, the absorbed dose-to-water at the reference point in the presence of a magnetic field is different than the dose without a magnetic field. To account for this difference the following dose conversion factor  is introduced;
is introduced;

where  is the absorbed dose-to-water for beam quality
is the absorbed dose-to-water for beam quality  in a magnetic field
in a magnetic field  at the same reference point as the absorbed dose-to-water without the magnetic field
at the same reference point as the absorbed dose-to-water without the magnetic field  . Note that the conversion factor accounts for the change of dose deposition in water because of the magnetic field and is therefore dependent on the magnetic field strength and its orientation relative to the photon field. Therefore the magnetic field is denoted as a vector. Note that this conversion factor is independent of the dosimeter.
. Note that the conversion factor accounts for the change of dose deposition in water because of the magnetic field and is therefore dependent on the magnetic field strength and its orientation relative to the photon field. Therefore the magnetic field is denoted as a vector. Note that this conversion factor is independent of the dosimeter.
Besides the fact that the change in local dose influences the reading of the ionization chamber, the magnetic field also influences the charge collection directly. Due to the presence of the magnetic field the electron trajectories will change, especially in lower density media such as an air-filled ionization chamber. As a result, the electron fluence inside and just around the chamber, and therefore the raw chamber reading, will change. The Bragg–Gray cavity conditions are therefore no longer valid and the dose-to-water cannot be determined directly from the chamber reading. Therefore a correction factor has to be applied to the chamber reading to take into account this effect. This correction factor  is defined as
is defined as

where  is the corrected raw reading without a magnetic field and
is the corrected raw reading without a magnetic field and  is the corrected raw reading (
is the corrected raw reading ( ) obtained in the presence of a magnetic field (equation (2)).
) obtained in the presence of a magnetic field (equation (2)).
The standard formalism can be adapted for the influence of the magnetic field using the dose conversion factor  and the correction on the detector reading
and the correction on the detector reading  . The dose-to-water in the presence of a magnetic field
. The dose-to-water in the presence of a magnetic field  is therefore
is therefore
Note that if we combine the  and the
and the  into a single correction factor this results in
into a single correction factor this results in
Where  is a modification of the
is a modification of the  factor which takes into account the change in
factor which takes into account the change in  due to the presence of the magnetic field. The
due to the presence of the magnetic field. The  factor was used in the formalism presented by O'Brien et al (2016) and determined by Monte Carlo. It can also be measured using calorimetry (de Prez et al 2016b). Using the relation above (equation (6)) the various methods to determine
factor was used in the formalism presented by O'Brien et al (2016) and determined by Monte Carlo. It can also be measured using calorimetry (de Prez et al 2016b). Using the relation above (equation (6)) the various methods to determine  can be compared.
can be compared.
To use the presented formalism to determine the absorbed dose under reference conditions, all factors in equation (5) should be established, including the two factors  and
and  . The
. The  is obtained via standard calibration procedures at a Standard Laboratory. The beam quality, Q, is specified by the tissue phantom ratio TPR20,10, which is then used to determine
is obtained via standard calibration procedures at a Standard Laboratory. The beam quality, Q, is specified by the tissue phantom ratio TPR20,10, which is then used to determine  (Andreo et al 2000, Aalbers et al 2008). The effects of recombination and polarity have to be verified for the specified beam quality in a magnetic field to correct the raw reading (Smit et al 2013).
(Andreo et al 2000, Aalbers et al 2008). The effects of recombination and polarity have to be verified for the specified beam quality in a magnetic field to correct the raw reading (Smit et al 2013).
The  and
and  factors are determined for an open beam in a region of transient charged particle equilibrium, i.e. on the central axis at depth below the depth of the dose maximum and the range of contamination electrons. The change in dose-to-water,
factors are determined for an open beam in a region of transient charged particle equilibrium, i.e. on the central axis at depth below the depth of the dose maximum and the range of contamination electrons. The change in dose-to-water,  , is best determined with Monte Carlo simulations of dose distributions in water, since the change in dose due to the magnetic field is small and therefore difficult to measure, and difficult to distinguish from the change in chamber response due to the magnetic fields. Only depth dose curves have to be simulated to determine
, is best determined with Monte Carlo simulations of dose distributions in water, since the change in dose due to the magnetic field is small and therefore difficult to measure, and difficult to distinguish from the change in chamber response due to the magnetic fields. Only depth dose curves have to be simulated to determine  and full representation of the detector is not required for these Monte Carlo simulations. Note that
and full representation of the detector is not required for these Monte Carlo simulations. Note that  is independent of the detector used. The change in local dose, is however, dependent on the orientations of the magnetic field and photon beam and on the beam energy spectrum. Therefore,
is independent of the detector used. The change in local dose, is however, dependent on the orientations of the magnetic field and photon beam and on the beam energy spectrum. Therefore,  has to be determined for the specific magnetic field orientation and beam quality used.
has to be determined for the specific magnetic field orientation and beam quality used.
The  factor can be determined for each detector used for reference dosimetry by measuring the reading with and without a magnetic field. Both the
factor can be determined for each detector used for reference dosimetry by measuring the reading with and without a magnetic field. Both the  and
and  depend on the orientation of the magnetic field and photon field and on the beam quality, but the
depend on the orientation of the magnetic field and photon field and on the beam quality, but the  factor is also specific to the detector design and the relative orientation of the chamber to both the magnetic field and the radiation beam. As a result the
factor is also specific to the detector design and the relative orientation of the chamber to both the magnetic field and the radiation beam. As a result the  factor has to be determined for the specific photon beam quality, magnetic field and detector orientation.
factor has to be determined for the specific photon beam quality, magnetic field and detector orientation.
3. Methods
3.1. MRI-Linac system and reference setup
This formalism was implemented in a protocol for reference dosimetry on the MRI-Linac installed at our department. The MRI-Linac (Elekta AB, Stokholm, Sweden) combines a 1.5 T MRI scanner (Philips Medical Systems, Best, the Netherlands) with a 7 MV linear accelerator. The magnetic field is directed out of the bore (i.e. along the IEC 1217, -y-axis) and is therefore orthogonal to the beam direction. The source to isocenter distance of this system is 143.5 cm.
The beam quality was quantified by the tissue-phantom ratio at depths of 20 and 10 cm (TPR20,10), for field size of 10 × 10 cm2 (Aalbers et al 2008) and was determined with and without the magnetic field. For this measurement the ionization chamber was positioned with its stem parallel to the magnetic field at the isocenter in an MRI-compatible version of the MP1 phantom (PTW GmbH, Freiburg, Germany). The MP1 phantom is a cuboid water tank with dimension 37 × 32 × 32 cm3 designed for absolute dose and beam quality measurements. The phantom size meets the requirements of the existing codes of practice on reference dosimetry (Almond et al 1999, Andreo et al 2000, Aalbers et al 2008).
For the other measurements and calculations, phantoms were positioned at a source to surface distance of 133.5 cm and a field size of 10 × 10 cm2 at isocenter was used. This is considered the reference setup. For the measurements, the orientation of the detector is described in section 3.3.
3.2. Dose-to-water Monte Carlo calculations
For the calculation of  , the GPUMCD Monte Carlo algorithm (Hissoiny et al 2011a, 2011b) was used to calculate the dose in water with and without magnetic field for the same reference setup. This model was validated against GEANT4 for dose calculation of radiotherapy beams (Hissoiny et al 2011a, Ahmad et al 2016). Calculations were performed using the reference setup for a water phantom of 40 × 40 × 35 cm3. The phantom size meets the requirements of the existing codes of practice on reference dosimetry (Almond et al 1999, Andreo et al 2000, Aalbers et al 2008). To illustrate the variation in dose due to the magnetic field,
, the GPUMCD Monte Carlo algorithm (Hissoiny et al 2011a, 2011b) was used to calculate the dose in water with and without magnetic field for the same reference setup. This model was validated against GEANT4 for dose calculation of radiotherapy beams (Hissoiny et al 2011a, Ahmad et al 2016). Calculations were performed using the reference setup for a water phantom of 40 × 40 × 35 cm3. The phantom size meets the requirements of the existing codes of practice on reference dosimetry (Almond et al 1999, Andreo et al 2000, Aalbers et al 2008). To illustrate the variation in dose due to the magnetic field,  was calculated for various field strengths of 0, 0.2, 0.35, 0.5, 0.7, 1, 1.2, 1.5, 2 and 3 T. For each magnetic field strength calculations were performed using a 1 mm grid size and a dose uncertainty of 1%. Based on this dose uncertainty the total number of particles is predicted by software to achieve the desired uncertainty in the central high dose region. To further reduce the statistical uncertainty, each depth dose curve was calculated 13 times.
was calculated for various field strengths of 0, 0.2, 0.35, 0.5, 0.7, 1, 1.2, 1.5, 2 and 3 T. For each magnetic field strength calculations were performed using a 1 mm grid size and a dose uncertainty of 1%. Based on this dose uncertainty the total number of particles is predicted by software to achieve the desired uncertainty in the central high dose region. To further reduce the statistical uncertainty, each depth dose curve was calculated 13 times.
Next, the mean depth dose curve along the central axes of these 13 calculations was determined, resulting in one depth dose curve for each magnetic field strength. Subsequently the mean depth dose curves were divided by the 0 T depth dose curve to illustrate the magnetic field effect on the central axis. To determine  the change in dose was determined by calculating the overall mean percentage difference at depths ranging from 6 to 15 cm to further reduce the uncertainty. The percentage difference of the dose for this range is nearly constant (O'Brien et al 2016). To indicate the uncertainty in the reduction in local dose and in
the change in dose was determined by calculating the overall mean percentage difference at depths ranging from 6 to 15 cm to further reduce the uncertainty. The percentage difference of the dose for this range is nearly constant (O'Brien et al 2016). To indicate the uncertainty in the reduction in local dose and in  , the standard error of the mean (SEM) was calculated.
, the standard error of the mean (SEM) was calculated.
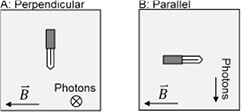
3.3. Detector response measurements on the MRI-Linac
The measurements for reference dosimetry were performed in a water phantom as described by Smit et al (2013). For the measurements the reference setup was used. The point of measurement was located in the isocenter of the beam (SAD = 143.5 cm) at a depth of 10 cm and 100 MU was delivered for each measurement. The  was determined for two ionization chamber orientations and for two different farmer type waterproof ionization chambers, the PTW 30013 (PTW GmbH, Freiburg Germany) and IBA FC65-G (IBA Dosimetry GmbH, Schwarzenbruck Germany). The chambers were aligned both perpendicular and parallel to the magnetic field and were always perpendicular to the photon field (figure 2). To prevent variations in reading due to air around the ionization chamber in the holders of standard solid water dosimetry phantoms, all measurements were performed in water using the waterproof ionization chambers (Hackett et al 2016, O'Brien et al 2017, Malkov and Rogers 2017b). Measurements were made with PTW Unidos electrometers (types T10022 and T10009). Measurements were performed before and after multiple ramp up and ramp down sessions of the magnetic field. Readings of the ionization chambers were corrected for temperature and pressure. Other correction factors, like saturation correction, are considered equal with and without the magnetic field (Smit et al 2013).
was determined for two ionization chamber orientations and for two different farmer type waterproof ionization chambers, the PTW 30013 (PTW GmbH, Freiburg Germany) and IBA FC65-G (IBA Dosimetry GmbH, Schwarzenbruck Germany). The chambers were aligned both perpendicular and parallel to the magnetic field and were always perpendicular to the photon field (figure 2). To prevent variations in reading due to air around the ionization chamber in the holders of standard solid water dosimetry phantoms, all measurements were performed in water using the waterproof ionization chambers (Hackett et al 2016, O'Brien et al 2017, Malkov and Rogers 2017b). Measurements were made with PTW Unidos electrometers (types T10022 and T10009). Measurements were performed before and after multiple ramp up and ramp down sessions of the magnetic field. Readings of the ionization chambers were corrected for temperature and pressure. Other correction factors, like saturation correction, are considered equal with and without the magnetic field (Smit et al 2013).
Figure 2. Orientation of the ionization chamber relative to the photon field and the magnetic field for the perpendicular and parallel orientation.
Download figure:
Standard image High-resolution imageIn order to position the chambers perpendicular to both the magnetic field and the photon beam (figure 2) a 20 × 20 × 10 cm3 water block phantom (phantom T41014, PTW, Freiburg, GmbH, Germany), which accommodates a farmer sleeve at a fixed depth of 5 cm. The sleeve was perforated to allow water around the ionization chamber. The gantry was rotated to 90° and the water block was put on its side with the opening at the top to prevent water leakage from the phantom. To measure at a depth of 10 cm, 5 cm of RW3 slabs (PTW, Freiburg, GmbH, Germany) were positioned on the side of the phantom through which the beam entered.
The measurements in which the ionization chamber was parallel to the magnetic field (figure 2) were performed with an MRI compatible version of the MP1 phantom (PTW GmbH, Freiburg, Germany).
4. Results
4.1. Beam quality
The beam quality measured at the MRI-Linac did not appear to be affected by the magnetic field. The measured TPR20,10 with magnetic field was 0.701 ± 0.002 (1 SD) and 0.700 ± 0.002 (1 SD) without magnetic field. The parameter TPR20,10 is in general practically independent of the SSD (Khan 2014), and this was verified for a range of SSDs including the SSD used in these experiments. Since there were no effects of the magnetic field on the beam quality the beam quality dependence  was determined using a standard code of practice (Aalbers et al 2008).
was determined using a standard code of practice (Aalbers et al 2008).
4.2. Difference in dose to water: 
The dose-to-water decreased with increasing magnetic field strength (figure 3). For a standard reference field size of 10 × 10 cm2 the decrease in dose was 0.51% ± 0.03% (1 SEM) at a magnetic field strength of 1.5 T, compared to the same setup without magnetic field. This resulted in a  factor of 0.9949 for that setup.
factor of 0.9949 for that setup.
Figure 3. The dose deviation for various magnetic field strengths relative to the dose without the presence of the magnetic field. The magnetic field was orientated orthogonal to the photon field axis. Error bars indicate the standard error of the mean.
Download figure:
Standard image High-resolution image4.3. Measurement of 
The presence of the magnetic field increased the readings of the PTW 30013 and the IBA FC65-G ionization chambers by 3.4% and 4.5% respectively when the ionization chamber was positioned orthogonal to the magnetic field and the photon beam. When the ionization chamber was positioned parallel to the magnetic field and orthogonal to the photon field the reading showed little change (<0.3%) relative to the reading without a magnetic field. The resulting  factors are shown in table 1.
factors are shown in table 1.
Table 1. The measured  and
and  for two ionization chambers positioned orthogonal and parallel to the magnetic field including the standard error of the mean. Also the number of measurement series, i.e. number of ramp ups and ramp downs of the magnetic field, (n) is given.
for two ionization chambers positioned orthogonal and parallel to the magnetic field including the standard error of the mean. Also the number of measurement series, i.e. number of ramp ups and ramp downs of the magnetic field, (n) is given.
| Chamber type |  |
 |
 |
 |
|---|---|---|---|---|
| PTW 30013 | 0.967 ± 0.002 | 5 | 0.997 ± 0.002 | 5 |
| IBA FC65-G | 0.957 ± 0.002 | 4 | 1.002 ± 0.003 | 5 |
5. Discussion
In this article we propose a formalism for reference dosimetry which can be used for radiotherapy in photon beams in the presence of a magnetic field. The difference to other formalisms is that the effects of the magnetic field on the dose distribution and on the reading of the dosimeter are taken into account separately. To demonstrate the use of the formalism in a protocol both of the effects are determined for the Elekta MRI-Linac, i.e. with the 1.5 T magnetic field orthogonal to the photon beam and for a nominal beam energy of 7 MV.
The effect of the magnetic field on the absorbed dose at a fixed depth has been determined here for multiple magnetic field strengths. In these simulations, the magnetic field was orthogonal to the photon beam. For this case the electrons released by photon–electron interactions travelled less in the forward direction since the electron paths were curved due to the Lorentz force. Therefore the energy was also released closer to the photon interaction point and the dose downstream decreased. This was especially the case for higher magnetic field strengths. For the same magnetic field orientation and a magnetic field strength of 1.5 T, O'Brien et al (2016) found with Monte Carlo simulation a reduction of 0.5% ± 0.1% of the dose-to-water. This result is in good agreement with the results found in this study. In another Monte Carlo study, Spindeldreier et al (2017) reported a reduction in dose of 0.3% for a 1 T magnetic field orientated orthogonal to a 6 MV photon beam, which is also consistent with the data reported in this article.
The change in response of the Farmer chambers due to the influence of the magnetic field was 3.4%–4.5% for the chamber aligned orthogonal to both the 1.5 T magnetic field and the photon beam. For the chamber aligned with the 1.5 T magnetic field the change in response was small (<0.3%). Similar findings were reported in previous studies (Meijsing et al 2009, Reynolds et al 2013, Smit et al 2013, Spindeldreier et al 2017). Due to the magnetic field, the path of the high energy electrons in the active volume of the ionization chamber can change and therefore result in more or in fewer ionizations, depending on the relative orientations of the chamber and magnetic field. The influx of these electrons can also change since the magnetic field alters the trajectories of the electrons. The net effect will be specific to the orientation of the chamber relative to the magnetic field and the photon field, and the magnetic field strength.
In order to compare our results to the results of other studies, the  factors for this study were also calculated. The
factors for this study were also calculated. The  and
and  are calculated based on the values of
are calculated based on the values of  ,
,  and
and  found in this study. The results are listed in table 2 together with the published data of other studies.
found in this study. The results are listed in table 2 together with the published data of other studies.
Table 2. The  and
and  of the UMC Utrecht data compared with the reported data in the literature based on measurements (M) and Monte Carlo (MC) calculations for two ionization chamber models. Uncertainties are shown between brackets as the least significant digit of the reported value. All uncertainties are of Type A, i.e. based on statistical methods only, except for de Prez et al, which includes Type B errors as well.
of the UMC Utrecht data compared with the reported data in the literature based on measurements (M) and Monte Carlo (MC) calculations for two ionization chamber models. Uncertainties are shown between brackets as the least significant digit of the reported value. All uncertainties are of Type A, i.e. based on statistical methods only, except for de Prez et al, which includes Type B errors as well.
| Chamber type | Reference | TPR20,10 |  |
 |
|
|---|---|---|---|---|---|
| PTW 30013 | UMC Utrecht | M | 0.701 | 0.963(2) | 0.992(2) |
| de Prez et al (2016b) | M | 0.702 | 0.961(7) | ||
| O'Brien et al (2016) | MC | 0.695 | 0.976(1) | 0.994(1) | |
| 0.961(1) |
|||||
| Malkov et al (2017a) | MC | 0.695 | 0.988(1) | ||
| Spindeldreier et al (2017) | MC | 0.674 | 0.954(3) | 0.993(3) | |
| 0.959(3) |
|||||
| IBA FC65-G | UMC Utrecht | M | 0.701 | 0.952(2) | 0.997(3) |
| de Prez et al (2016b) | M | 0.702 | 0.951(7) | ||
| Malkov et al (2017a) | MC | 0.695 | 0.992(1) | ||
aResult obtained with chamber in the perpendicular orientation as shown in figure 2, but with the magnetic field in the opposite direction.
For the parallel orientation the measurement based  values determined in this study are well in agreement (<0.5%) with the Monte Carlo based studies for both the PTW chamber (O'Brien et al 2016, Spindeldreier et al 2017, Malkov and Rogers 2017a) and the IBA chamber (Malkov and Rogers 2017a). Furthermore, the correction needed for the parallel orientation of the ionization chamber is smaller than that for the perpendicular orientation. For chambers in the perpendicular orientation, the results are in good agreement (0.2% difference) with the results of de Prez et al (2016b), who measured the
values determined in this study are well in agreement (<0.5%) with the Monte Carlo based studies for both the PTW chamber (O'Brien et al 2016, Spindeldreier et al 2017, Malkov and Rogers 2017a) and the IBA chamber (Malkov and Rogers 2017a). Furthermore, the correction needed for the parallel orientation of the ionization chamber is smaller than that for the perpendicular orientation. For chambers in the perpendicular orientation, the results are in good agreement (0.2% difference) with the results of de Prez et al (2016b), who measured the  factor directly in a magnetic field using a calorimeter (de Prez et al 2016a) for both ionization chambers. The
factor directly in a magnetic field using a calorimeter (de Prez et al 2016a) for both ionization chambers. The  factor was also calculated using Monte Carlo for the PTW chamber. The variation between the
factor was also calculated using Monte Carlo for the PTW chamber. The variation between the  values in these studies and the measurement-based
values in these studies and the measurement-based  values is, however, larger than the variation found for the parallel orientation. Also, the measurement-based
values is, however, larger than the variation found for the parallel orientation. Also, the measurement-based  values are closer to the
values are closer to the  values calculated with the magnetic field in the opposite direction. Furthermore, the effect of the magnetic field orientation when the chamber is perpendicularly oriented to the magnetic field is much larger, and in the opposite direction, in the study of O'Brien et al than in the study of Spindeldreier et al. The influence of the magnetic field on ionization chamber measurements may be more difficult to accurately simulate with Monte Carlo, and therefore the parallel orientation is more preferable for reference dosimetry. The effective sensitive volume has an important impact on the chamber response in Monte Carlo simulations (Spindeldreier et al 2017, Malkov and Rogers 2017a, 2017b). The charge collecting electric field inside the chamber can be distorted, especially near the guard electrode, and charge released in this volume may not be collected. The influence of the effective sensitive volume on the change of chamber response due to the magnetic field depends on the orientation of the magnetic field, photon beam and chamber.
values calculated with the magnetic field in the opposite direction. Furthermore, the effect of the magnetic field orientation when the chamber is perpendicularly oriented to the magnetic field is much larger, and in the opposite direction, in the study of O'Brien et al than in the study of Spindeldreier et al. The influence of the magnetic field on ionization chamber measurements may be more difficult to accurately simulate with Monte Carlo, and therefore the parallel orientation is more preferable for reference dosimetry. The effective sensitive volume has an important impact on the chamber response in Monte Carlo simulations (Spindeldreier et al 2017, Malkov and Rogers 2017a, 2017b). The charge collecting electric field inside the chamber can be distorted, especially near the guard electrode, and charge released in this volume may not be collected. The influence of the effective sensitive volume on the change of chamber response due to the magnetic field depends on the orientation of the magnetic field, photon beam and chamber.
In the proposed formalism, the effect of the magnetic field on the dose distribution and on the reading of the dosimeter are taken into account as two distinct factors,  and
and  . O'Brien et al (2016) presented a different formalism using
. O'Brien et al (2016) presented a different formalism using  as a correction of the
as a correction of the  factor to determine the dose in presence of a magnetic field. Malkov and Rogers (2017a) used another approach, which combines the standard beam quality correction and the magnetic field corrections in a single factor to directly correct the
factor to determine the dose in presence of a magnetic field. Malkov and Rogers (2017a) used another approach, which combines the standard beam quality correction and the magnetic field corrections in a single factor to directly correct the  , calibration factor, i.e. a correction of the absorbed dose-to-water coefficient for the reference beam quality. The factors used by O'Brien et al and Malkov et al can only be determined directly by primary absorbed dose to water standards, such as e.g. calorimeters (de Prez et al 2016a), or by Monte Carlo simulations of the ionization chamber used for reference dosimetry. Absorbed dose to water primary standards which can operate in a magnetic field are, however, not widely available. Detailed Monte Carlo simulations have been performed only for specific models of ionization chambers and variations between chambers of the same type have not yet been investigated. Furthermore, Monte Carlo simulations have to be verified against measurements, for example to incorporate the influence of the effective sensitive volume. The proposed formalism enables radiotherapy departments to determine the correction factors required for reference dosimetry in a magnetic field, by separating the effects on the dose distribution and the response of the chamber. The
, calibration factor, i.e. a correction of the absorbed dose-to-water coefficient for the reference beam quality. The factors used by O'Brien et al and Malkov et al can only be determined directly by primary absorbed dose to water standards, such as e.g. calorimeters (de Prez et al 2016a), or by Monte Carlo simulations of the ionization chamber used for reference dosimetry. Absorbed dose to water primary standards which can operate in a magnetic field are, however, not widely available. Detailed Monte Carlo simulations have been performed only for specific models of ionization chambers and variations between chambers of the same type have not yet been investigated. Furthermore, Monte Carlo simulations have to be verified against measurements, for example to incorporate the influence of the effective sensitive volume. The proposed formalism enables radiotherapy departments to determine the correction factors required for reference dosimetry in a magnetic field, by separating the effects on the dose distribution and the response of the chamber. The  factor can be determined by Monte Carlo simulation of dose distributions in water. As only the change in local dose has be determined, the details of the ionization chamber are not necessary, which simplifies the simulations. The change in detector reading due to the magnetic field,
factor can be determined by Monte Carlo simulation of dose distributions in water. As only the change in local dose has be determined, the details of the ionization chamber are not necessary, which simplifies the simulations. The change in detector reading due to the magnetic field,  , can be determined relatively easily from measurements for any detector and for all orientations during ramp-up or ramp-down procedures. The advantage is that this measurement in principle can be performed at a department during for example a ramp up procedure at the time of installation. The proposed formalism would therefore also be useful for detector development since the correction factors can be determined locally. Finally the presented formalism can be used to independently verify
, can be determined relatively easily from measurements for any detector and for all orientations during ramp-up or ramp-down procedures. The advantage is that this measurement in principle can be performed at a department during for example a ramp up procedure at the time of installation. The proposed formalism would therefore also be useful for detector development since the correction factors can be determined locally. Finally the presented formalism can be used to independently verify  factors that are determined from calorimetry measurements or Monte Carlo simulations.
factors that are determined from calorimetry measurements or Monte Carlo simulations.
6. Conclusions
A new formalism is proposed for reference dosimetry in the presence of magnetic fields. In this formalism the effect of the magnetic field on the dose distribution and the detector reading are separated. The measurements can be performed by individual departments and the formalism can be used to determine the correction factors needed to establish the absorbed dose in a magnetic field. This protocol was implemented for clinical use at our department.
Acknowledgments
This work was partially funded by EURAMET through EMPIR grant 15HLT08 MRgRT.