Abstract
Current noninvasive blood pressure (BP) measurement methods, such as the oscillometric method, estimate the systolic and diastolic blood pressure (SBP and DBP) at two random instants in time and do not take into account the natural variability in BP. The standard for automated BP devices sets a maximum allowable system error of ±5 mmHg, even though natural BP variability often exceeds these limits. This paper proposes a new approach using simultaneous recordings of the oscillometric and continuous arterial pulse waveforms to augment the conventional noninvasive measurement by providing (1) the mean SBP and DBP over the measurement interval and the associated confidence intervals of the mean, (2) the standard deviation of SBP and DBP over the measurement interval, which indicates the degree of fluctuation in BP and (3) an indicator as to whether or not the oscillometric reading is an outlier. Recordings with healthy subjects demonstrate the potential utility of this approach to characterize BP, to detect outlier measurements, and that it does not suffer from bias relative to the conventional oscillometric method.
Export citation and abstract BibTeX RIS
For more information on this article, see medicalphysicsweb.org
1. Introduction
Blood pressure (BP) is an important vital sign and a very commonly measured physiological parameter in clinical practice (Avolio et al 2010). The maximum and minimum of the arterial BP pulse, known as the systolic and diastolic blood pressure (SBP and DBP), are the two values that are usually used to characterize BP (Webster 1998). Intermittent noninvasive automatic measurement of SBP and DBP is widely used in a broad variety of clinical settings and in home health monitoring (O'Brien et al 2001). The BP signal, however, is characterized by continuous fluctuations, and so the SBP and DBP are subject to significant continuous changes over time. Nevertheless, typically SBP and DBP are estimated at two random time instances, which do not provide information on the significant fluctuations in BP. A recent editorial in the journal Hypertension of the American Heart Association asserts that this is a serious deficiency in current measurement techniques: 'few measurements in medicine are made as poorly and inconsistently as BP measurement. Methods used today in clinical practice and in clinical trials are little changed from the earliest days of measurement. Although there is a clear recognition of biological variability, we continue to make decisions largely upon measurements taken at random times under poorly controlled conditions' (Jones and Hall 2008).
The estimation of BP using available automated devices is subject to large measurement uncertainty. For example, in one study it was shown that the BP values provided by patients' devices differed from those obtained using the conventional auscultatory method by more than 5 mmHg in approximately 50% and 40% of the measurements, for SBP and DBP, respectively (Cuspidi et al 2005). According to the ANSI/AAMI SP10 standard, the maximum accepted error of an automated sphygmomanometer is limited to ±5 mmHg relative to reference readings taken simultaneously by at least two trained operators with a calibrated manometer (AAMI/ANSI-SP10 2002), although the measurements with the automated devices and trained operators need not be concurrent. However, intrinsic physiological oscillations of the BP signal can lead to shifts of up to 20 mmHg in both the SBP and DBP within a few heartbeats (Hansen et al 2006). Therefore, the estimation of BP is subject to two sources of uncertainty: the first due to measurement system inaccuracy and the second due to physiological variability. BP measurement standards, such as the ANSI/AAMI SP10, limit the uncertainty introduced by measurement error but do not address the contribution of the physiological variability to estimation uncertainty (Jones and Hall 2008). The question remains as to whether uncertainty in the BP estimate poses a problem for diagnosing and treating hypertension. The editorial in Hypertension states that 'although some might argue that a 3–4 mmHg increase in BP is not clinically significant, clinical trials and population studies remind us of the importance of these seemingly small changes' (Jones and Hall 2008). A recent 1 million-patient meta-analysis suggests that a 3–4 mmHg systolic increase in BP would translate into 20% higher stroke mortality and a 12% higher mortality from ischemic heart disease (Lewington et al 2002).
This paper presents an approach to augment the conventional automated measurement of BP by taking into account physiological variability. BP variability is principally determined by the sympathovagal balance of cardiovascular regulation (Laitinen et al 1999). It can be studied over various time scales ranging from seconds to years (e.g. Ando et al 1997, Hansen et al 2006), and investigated using SBP and DBP measurements or a continuous recording of the arterial pulse waveform. The proposed approach involves simultaneously collecting the continuous arterial pulse waveform from one arm and the oscillometric waveform (OMW) from the other arm, over 90 s. The OMW is commonly used to derive the SBP and DBP in automated BP devices (Moraes et al 1999). The continuous arterial pulse waveform can be obtained noninvasively using different readily available techniques such as tonometry or optical plethysmography, although in this work it is obtained by applying constant pressure in a cuff, connected to a piezoelectric transducer. Combining the information from the OMW and the continuous pulse waveform provides three measures that augment the conventional BP readings. (1) The means of SBP and DBP over the measurement interval and associated confidence intervals. These values are arguably more representative of the BP than the oscillometric values obtained at two random instants in time. (2) The standard deviation of SBP and DBP over the interval which gives information about BP variability. (3) And whether or not the oscillometric readings are outliers relative to the distribution of the readings over the interval, a finding which could be used to generate an alert (e.g. to repeat the measurement).
The proposed approach was tested over several measurements in healthy subjects and compared to the conventional oscillometric approach. Furthermore, in order to characterize the uncertainty introduced by the BP variability, the percentage of SBP and DBP beats in all subjects that exceeds ±5 mmHg relative to the mean value over the recording interval was calculated. This percentage allowed a direct comparison between the uncertainties introduced by the measurement inaccuracy and the biological variability, respectively. As part of the analysis, we also sought to identify the percentage of beats that would lead to 'outlier' readings of SBP and DBP, in the measurement interval.
2. Methods
2.1. Subjects
Fifteen adults (seven male and eight female subjects, age ranging from 19 to 50 years) with no known history of heart disease participated in this study. All subjects provided informed consent prior to the measurement, in accordance with the guidelines of the Institutional Research Ethics Board.
2.2. Measurement system
We developed a BP measurement unit that includes two pressure cuffs, each connected to an analog pressure transducer. An illustrative block diagram is shown in figure 1. The Vernier pressure transducer (SenSym SDX05D4, Beaverton, OR, USA) and National InstrumentsTM (Austin, TX, USA) hardware and software are used to acquire the arterial pulse wave data from the two arms. The Vernier pressure transducer operates on a dc supply voltage of 5 V and converts the mechanical vibrations exerted by the blood circulation on the cuff to an analog output voltage signal in the range of 0–5 V. The conversion factor is 56.11 mmHg V−1.
Figure 1. Illustrative block diagram of the measurement set-up and device.
Download figure:
Standard imageA first BP cuff is placed on the subject's upper left arm and is inflated to a constant pressure, using a manual pump, and is employed to retrieve the continuous arterial pulse waveform. A second BP cuff is placed on the upper right arm and controlled by an automatic 6 V dc mini air pump. The pump operates with a pushbutton mounted on the prototype; once pressed, the button turns the pump on and the brachial cuff is gradually inflated and then deflated to conduct the oscillometric measurement. A screw-controlled manual pressure release valve is connected in-line with the brachial cuff. The rotation of the screw determines the deflation rate of the cuff (Ahmad et al 2010).
The analog voltage outputs of the two transducers (corresponding to the two BP cuffs) are fed to two simultaneously sampled analog channels of the National InstrumentsTM C Series 9239 analog input module (NI-9239) mounted on a CompactDAQ data acquisition system. The analog signals are conditioned, buffered and then sampled, at a frequency (fs) of 1.613 kHz, by a 24 bit delta-sigma analog-to-digital converter. Prior to digitization, the signal passes through an in-built anti-aliasing filter on the data acquisition board with a cutoff frequency equal to 0.453fs. The quantized signals are then transmitted to a personal computer via a universal serial bus (USB) cable. The voltage supply to the Vernier pressure transducers is provided from a National InstrumentsTM C Series 9263 4-Channel, 16 bit, ± 10 V analog output module (NI-9263) also mounted on the CompactDAQ system.
National InstrumentsTM LabVIEW development environment is used for data acquisition of the constant pressure arterial waveform and the oscillometric BP signals. We developed a customized LabVIEW user interface that displays the acquired arterial pulse waveform and oscillometric signal data in real-time. Signal processing and statistical analysis are performed offline using Matlab® (The MathWorks Inc., Natick, MA, USA). To minimize the effects of 60 Hz contamination and other interferers, the signals were digitally filtered using a third-order FIR low-pass filter with a cutoff frequency of 30 Hz prior to further analysis.
2.3. Experimental procedure
The subject is comfortably seated and asked to relax with minimum movement. The first cuff is placed on the upper left arm for the constant cuff pressure arterial pulse waveform measurement, the second cuff is placed on the upper right arm for oscillometric inflation and an automated BP device (UFIT, Biosign Inc., Toronto, Canada) is placed on the wrist of the right arm. UFIT is a commercial device that uses a wrist cuff to estimate the systolic and diastolic BP. In a study on 87 participants, the manufacturer reports an error (mean ± SD) of 0.3 ± 6.9 mmHg for the systolic pressure and 0.2 ± 5.2 mmHg for the diastolic pressure, compared to measurements with two trained observers (Biosign report 2011), and so the device meets the performance requirements of the AAMI/ANSI-SP10 (2002) standard for automated sphygmomanometers. The UFIT device is used to find the systolic and diastolic values at the start of every recording, but its cuff is kept deflated for the remainder of the session, and does not play a further role in the measurement.
The cuff on the left arm is inflated to reach a constant pressure, close to the diastolic pressure of the subject determined by the UFIT device (DBP + 3 mmHg), which was the minimal pressure allowing a clear visual identification of the pulse while at the same time minimizing any discomfort. This applied pressure value was determined experimentally, and the detection algorithm was able to detect pulses while the BP varied throughout the whole measurement. Once the pressure in the cuff on the left arm reaches a constant value, an oscillometric measurement is made on the right arm. In this arm, the cuff is inflated to a pressure higher than the systolic pressure, determined by the UFIT device (SBP + 5 mmHg), and then slowly deflated. Acquisition of data from the two cuffs is triggered simultaneously by the control software, and lasts 90 s, with the constant pressure cuff providing the continuous arterial pulse waveform and the oscillometric cuff generating the SBP and DBP values. The appropriate interval over which the mean SBP or DBP should be estimated is not known; however, a duration in the range of 1–2 min is expected to include the major short-term physiological oscillations (Elghozi 2008).
A single experimental session consists of a reference reading using UFIT followed by a BP recording from the two arms (oscillometric and constant pressure), in parallel, with these two steps repeated five times. At the end of the session, an additional recording is performed on both arms in which the subject is asked to breathe deeply, at a rate of 8 s/breath (i.e. breathing frequency of 0.125 Hz). A software-generated metronome is set up on the monitor, during this recording, to help the subject maintain the required breathing frequency. Deep breathing is employed because it typically results in particularly large excursions in the arterial pulse waveform.
2.4. Waveform extraction
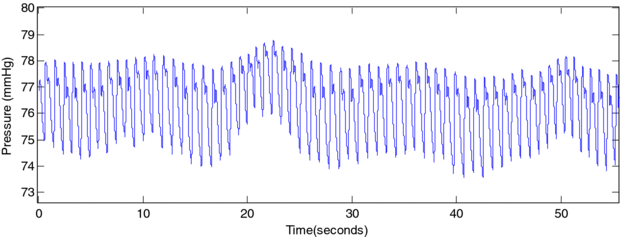
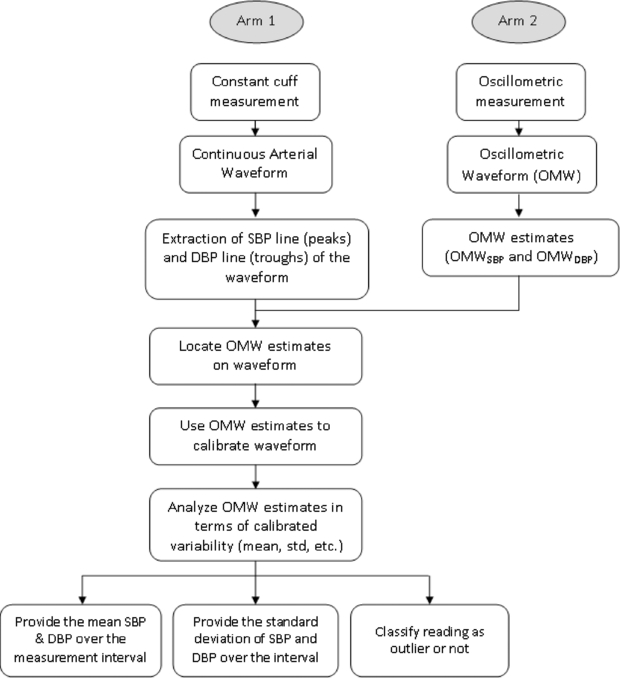
A block diagram of the proposed approach is shown in figure A1. A customized peak detection algorithm is applied to the two recorded signals in order to detect the peaks (systolic points) and troughs (diastolic points) of the pulse waveform. The peak detection algorithm is based on an existing method for ECG peak detection (Kohler et al 2003) with minor alterations compensating for the shape disparity between an ECG pulse and a BP pulse (Chen 2010). In the first iteration, the continuous pulse waveform (shown in figure 2) is filtered using a third-order IIR Butterworth band-pass filter applied with cutoffs at 0.25 and 2.5 Hz, with the signal fed forward and then backward. The upward and downward zero crossings are then detected in order to find the start and end of each pulse, and the peaks/troughs are identified. A second iteration uses the detected peaks to build a band-pass filter, centered at the heart rate frequency, calculated as the mean of the inter-peak intervals of the first iteration. The band-pass filter has cutoff frequencies at twice the standard deviation of the heart rate on each side, or HR − 2 × stdHR and HR + 2 × stdHR, with 'HR' being the heart rate and 'std HR' its standard deviation. The zero crossings are identified during the second iteration and the final peaks and troughs represent, once again, the maximum and minimum values in between the upward and downward crossings, respectively (Chen 2010).
Figure 2. Section of the uncalibrated continuous arterial pulse waveform. The uncalibrated pulse series represents the raw data (pressure detected by the sensor in the cuff, after inflating it to a constant pressure). The values fluctuate around the constant pressure value, due to the force exerted by the intra-arterial pressure pulses. In order to represent the intra-arterial pressure, these values need to be scaled by a factor calculated from the calibrated SBP and DBP values, obtained using the oscillometric measurement.
Download figure:
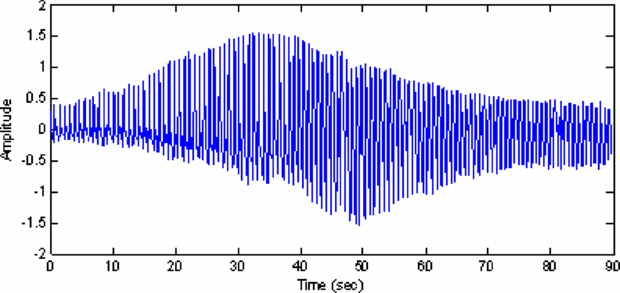
Standard imageA second-order high-pass Butterworth filter is applied to the OMW (shown in figure 3), with a cutoff frequency of 0.1 Hz. The filter suppresses the frequency components that are related to the slowly deflating cuff pressure and allows the remaining components of the signal to pass through (Geddes et al 1982, Sorvoja et al 2005). These components correspond to the subject's pressure pulses that form the desired OMW.
Figure 3. OMW obtained after high-pass filtering the deflating cuff waveform.
Download figure:
Standard imageOnce the OMW is extracted, the oscillometric pulse index (OPI) is defined as the area obtained by integrating each pulse (Jazbinsek et al 2005, Ball-llovera 2003, Gershak et al 2006). The OPI values are used to construct a signal envelope that is interpolated and resampled at 100 Hz (Chen 2010).
The maximum amplitude algorithm (MAA), which has been reported to be the most popular algorithm for determining BP from OMWs (Baker et al 1997), is used to estimate the SBP and DBP values. MAA requires, as a first step, finding the point on the envelope that corresponds to the mean arterial pressure (MAP), which is estimated to be the maximum point on the OPI. Locating this value on the deflation curve allows us to obtain the MAP value in mmHg. Once plotted on the OPI, the MAP virtually divides the envelope into two parts: the left part represents the systolic side and the right part becomes the diastolic side. The MAA algorithm then utilizes systolic and diastolic characteristic ratios, determined empirically in large-scale studies, to find the points that correspond to SBP and DBP. In the literature, the systolic ratio ranges from 0.45 to 0.73 and the diastolic ratio ranges from 0.69 to 0.83 depending on specifics of the applied MAA. The height (amplitude A) of the maximum point is multiplied by the systolic ratio (rs) and the diastolic ratio (rD) in order to obtain the amplitude of the systolic point (located on the systolic side) and the diastolic point (located on the diastolic side), respectively (equation (1)). The ratios used in this study are 0.55 and 0.8 for rs and rD, respectively, based on a previous study by Chen (2010):
Once the diastolic and systolic points are found on the envelope, they are mapped back to the deflation curve giving the SBP and DBP values in mmHg. The oscillometric algorithm explained in this section and used as the starting point of the proposed approach has been previously validated in our laboratory (Chen 2010).
2.5. SBP and DBP mapping and calibration
In the conventional oscillometric measurement, the systolic BP corresponds to a specific heartbeat: the beat at which the BP became higher than the deflating cuff pressure and the blood was capable of flowing in the brachial artery. This specific moment is accompanied with a well-identified Korotkoff sound that can be heard by trained observers using a stethoscope. Similarly, the diastolic BP also corresponds to a specific beat. This correspondence is the basis of the time mapping explained in this section.
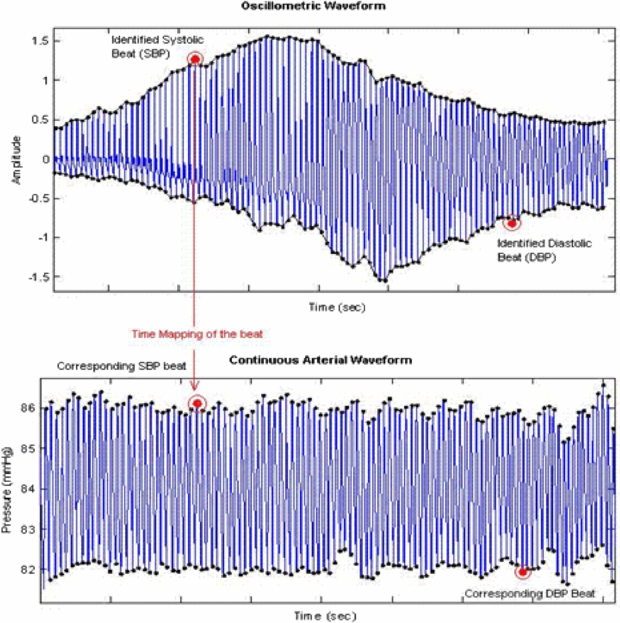
Following the execution of the peak detection algorithm, the estimated values of SBP and DBP on the interpolated envelope of the OMW are matched to the SBP and DBP beats in the continuous pulse waveform. This is done by finding the closest peak and trough to those values, respectively; the peak that is the closest to the SBP time point on the envelope is tagged as the SBP beat and the closest trough to the DBP time point on the envelope is tagged as the DBP beat. These points are then mapped to their respective corresponding beats on the constant pressure pulse waveform (figure 4).
Figure 4. The graph on top shows the OMW with the identified SBP and DBP peaks. The graph below shows the synchronous continuous recording taken at a constant pressure and the SBP and DBP peaks mapped from the OMW.
Download figure:
Standard imageThe final stage of the mapping consists of the calibration of the constant pressure pulse waveform, which is originally centered around the value of the external pressure applied by the cuff on the subject's arm. The calibration follows the equation
where OMWSBP and OMWDBP are the calibrated SBP and DBP values generated from the oscillometric method, uncalibratedSBP and uncalibratedDBP are the uncalibrated corresponding SBP and DBP points on the constant cuff pressure recording, and yuncalibrated and ycalibrated (both functions of the time variable 't') indicate a given point in the constant cuff pressure curve before and after calibration, respectively. This equation results in a calibrated continuous recording from which we can obtain the calibrated SBP and DBP values for the duration of the measurement as well as the estimation of calibrated means, standard deviations, ranges and histograms. It should be noted that the generation of the statistical profile of the SBP and DBP during the measurement would not be affected by the location of the oscillometric estimates relative to the mean.
2.6. Data analysis
The next step is to identify the uncertainty in the SBP and DBP estimates that result from BP variability, and to classify outlier values. Descriptive statistics and histograms were obtained using SPSS (IBM, NY, USA). In the analysis of heart rate variability, short duration signals of less than 5 min are assumed to be at least approximately stationary (Task Force of the European Society of Cardiology and the North American Society of Pacing Electrophysiology 1996). As a result, we also assumed that the signals we analyzed were approximately stationary, since they are considerably shorter than 5 min.
The mean of the SBP and DBP values in the continuous BP waveform over the 90 s measurement interval (INT_MEANSBP and INT_MEANDBP) is calculated. The standard deviation around these means is also calculated (INT_STDSBP and INT_STDSBP). The SBP and DBP points estimated from the oscillometric measurement (i.e. OMWSBP and OMWDBP) are identified on the SBP and DBP histograms, respectively, in order to determine whether or not they are outliers. Locating the oscillometric values relative to the histogram could alert the user that the reading is potentially over- or underestimating their BP (represented by the mean over the measurement interval) and notifying them that a second reading may be needed to validate the first one. The three additional parameters for each of the SBP and DBP pressures (INT_MEAN, INT_STD and outlier indicator) are used to augment the conventional oscillometric BP measurement using information about BP variability over the measurement interval. Paired t-tests and Bland–Altman plots are used to compare the new measures and the conventional oscillometric SBP and DBP readings (i.e. OMWSBP and OMWDBP) and were performed using Analyse-it® (Leeds, UK).
Over the 90 measurements taken from 15 subjects (six readings per subject), the percentage of oscillometric SBP and DBP values (i.e. OMWSBP and OMWDBP) (1) located beyond ±5 mmHg from the mean values over the interval and (2) located at a distance exceeding the (2× SD) margin was evaluated in order to assess the contribution of BP variability to measurement uncertainty (Barnett, 1994). The first criterion corresponds to the maximum device accuracy error accepted by the SP10 standard (AAMI/ANSI-SP10 2002) and the second is used to determine outliers. It should be noted, however, that the proposed approach is not tied to any one criterion used for determining outliers. The criterion we suggest is one that is commonly used, but other criteria that may be less sensitive to the effects of the outliers on the sample mean and SD, such a criterion based on the upper/lower quartile ±1.5 times the interquartile range, could also be used (Wilcox 2001).
2.7. Correlation between BP variability in right and left arms
Since mapping is made between beats in pulse pressure waveforms obtained from the two arms, it is important that the variability in the two arms be highly correlated. Therefore, a subsidiary experiment was conducted on the 15 subjects, where a cuff was placed on both arms and inflated to the same constant pressure (diastolic BP + 3 mmHg) for 60 s. There was a correlation of 98.59 ± 1.41% (mean ± standard deviation, range 90.49–99.9%, over 15 samples) between the interpolated peak line signals (for SBP and DBP) acquired from both arms. This suggests that, at least in healthy subjects, the variability of the pulse waveform is synchronized and very similar in both arms (Eguchi et al 2007).
3. Results
On average, over all subjects and trials, 15.7% of the SBP points and 14.6% of the DBP points are found to exceed ±5 mmHg from the mean values, the maximum device accuracy error accepted by the SP10 standard (AAMI/ANSI-SP10 2002). Furthermore, 11.24% of the SBP points and 4.49% of the DBP points exceed the (2× SD) margin, and may be considered outliers.
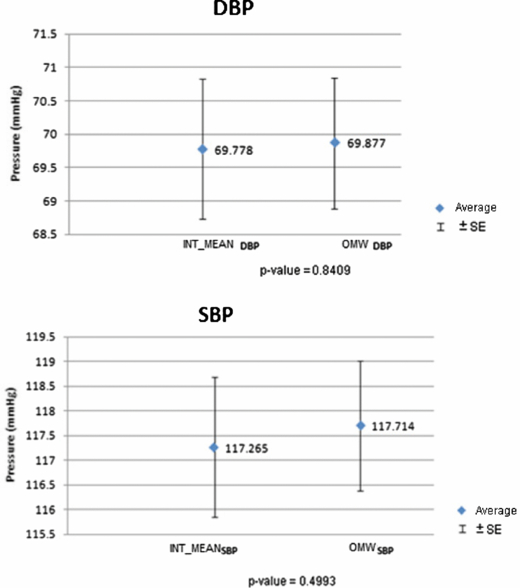
To compare the SBP and DBP obtained from the two measurement techniques (i.e. the value obtained using the conventional oscillometric method and the mean value over the interval reported by the proposed approach), we used a paired t-test on INT_MEAN and OMW values across data points from all subjects (figure A2). Since the oscillometric part of the approach went through verification in prior work and the output was comparable to the commercial device (Chen 2010), it was used as a reference in this study. The result of the t-test shows that there is no statistically significant difference between the means of the measurements obtained by the two approaches (p-values = 0.4993 for SBP and 0.8409 for DBP). The average INT_MEANSBP and INT_MEANDBP were 117.26 and 69.78 mmHg, respectively, and the average OMWSBP and OMWDBP were 117.71 and 69.88 mmHg, respectively (absolute mean difference = 0.449 mmHg for SBP and 0.099 mmHg for DBP). We can then conclude that the proposed method does not introduce additional errors to the estimates of SBP and DBP when assessed over all subjects and all trials. However, in an individual subject and in a given trial, the proposed method often gives estimates that are different from the ones obtained by conventional oscillometry. Since the conventional oscillometric reading is obtained at one instant in time, and the reading provided by the proposed method reflects an average over the measurement interval, such differences are to be expected.
Figure A1. Block diagram of the proposed approach for augmented BP measurement.
Download figure:
Standard imageFigure A2. Graphs showing the paired t-test results; average of the INT_MEANSBP ± SEM (standard error of the mean) and the OMWSBP ± SEM (top graph) and average of the INT_MEANDBP ± SEM and the OMWDBP ± SEM (bottom graph), across all subjects and all trials.
Download figure:
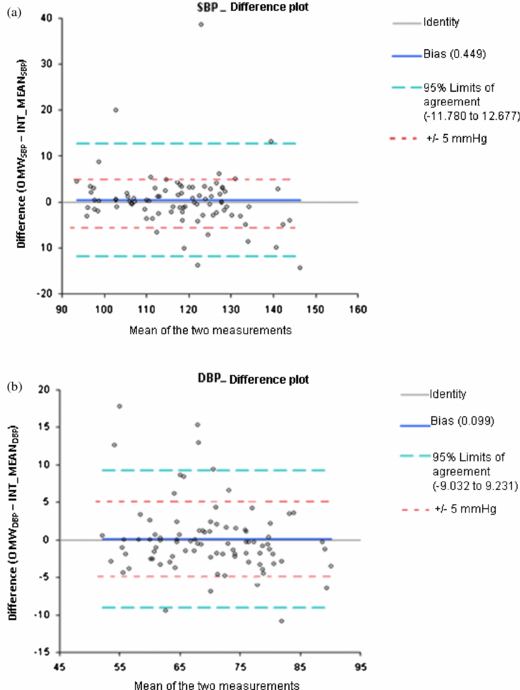
Standard imageIn order to gain further insight as to how well the two methods agree, a Bland–Altman test was performed. The OMWSBP and OMWDBP, over all subjects and trials, and the INT_MEANSBP and INT_MEANDBP calculated using the continuous waveform were the variables in the test. Figure A3 shows the Bland–Altman plots for both the SBP and DBP. The means of the two measures (i.e. of OMW and INT_MEAN) are plotted on the horizontal axis and the differences are plotted on the vertical axis, showing the amount of disagreement between the two measures, via the differences. The bias is equal to the absolute mean differences between the two measurement techniques as described above, and is very small for both SBP and DBP. The plots also indicate that the proposed method does not introduce a significant error trend compared to the oscillometric method. On the other hand, the 95% limits of agreement are located at about ±11 mmHg, which confirms that the two methods provide different results in individual trials. As mentioned above, such differences are to be expected. The Bland–Altman plots also show the outliers (in this case, values exceeding the 95% limits of agreement) and the points exceeding the ±5 mmHg margin relative to the mean over the interval.
Figure A3. Bland–Altman difference plots showing bias and limits of agreement between the SBP (a) and DBP (b) values estimated by the oscillometric method and the interval mean SBP and DBP values calculated using the constant cuff method.
Download figure:
Standard imageIn order to assess the reliability of the reported interval means (INT_MEANSBP and INT_MEANDPB), the 95% statistical confidence interval of the mean was calculated. According to the central limit theorem, the confidence interval with a confidence level of 95% (CI) can be defined as the mean ± 1.96× SD/√N, or approximately ±2× SD/√N (Rice 1995). Over the 15 subjects and over all trials, the average CIs were as follows: ± 0.99 mmHg (range 0.28–5.37 mmHg) for SBP and ± 0.98 mmHg (range 0.25–6.25 mmHg) for DBP. Therefore, on average, in a given trial, we can be confident that the actual interval mean for SBP and DBP falls within less than ± 1 mmHg relative to the reported interval mean, 95% of the time.
To illustrate how the proposed method provides augmented measures of BP, and show how it can be useful for detecting measurement outliers, sample readings in two different subjects are presented. Waveform graphs are shown for each case, the first identifying the measured beat in the continuous arterial pulse waveform, the second presenting the calibrated interpolated line (for SBP or DBP) and the third identifying where the measured oscillometric value falls within the histogram of the SBP or DBP values over the measurement interval. The graphs are followed by a table that includes the conventional oscillometric measurement, the three measures provided by the proposed method and observations on each case (figures A4–A7 and tables A1 and A2).
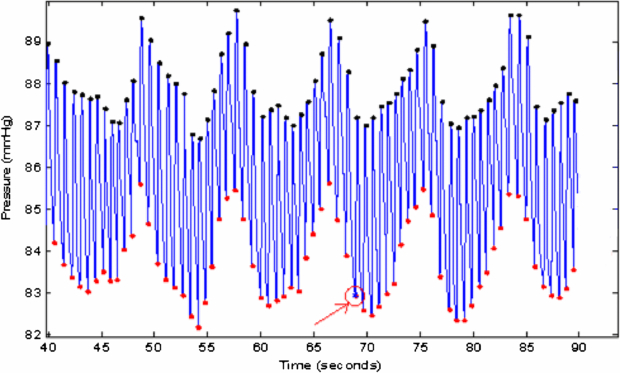
Figure A4. Case 1: example of DBP estimated by the oscillometric method at a low point, far below the DBP interval mean (INT_MEANDBP) during deep breathing (see also figure A5 and table A1). Zoomed-in portion of the continuous pulse waveform (between the 40th and 90th seconds), after applying the peak detection algorithm; the DBP measured using the oscillometric method is identified by the arrow and circle at around 69 s.
Download figure:
Standard imageFigure A5. Case 1: the calibrated interpolated line joining the troughs of the continuous recording, with the oscillometric diastolic point (DBP) represented as a star (*) on the waveform at around 69 s. The horizontal line in the center of the graph represents the INT_MEANDBP.
Download figure:
Standard imageFigure A6. Case 2: example of DBP estimated by the oscillometric method at a high point, far above the DBP interval mean (INT_MEANDBP) during normal breathing (see also figure A7 and table A2). Zoomed-in portion of the continuous pulse waveform (between the 45th and 92th seconds), after applying the peak detection algorithm; the DBP measured using the oscillometric method is identified by the arrow and circle at around 70 s.
Download figure:
Standard imageFigure A7. Case 2: the calibrated line joining the troughs of the continuous recording, with the identified systolic point (DBP) represented as a star (*) on the waveform at around 70 s. The horizontal line in the center of the graph represents the INT_MEANDBP.
Download figure:
Standard image4. Discussion and conclusions
BP is characterized by continuous fluctuations caused by various physiological factors. These fluctuations contribute to uncertainty in the estimation of systolic or diastolic blood pressure (SBP or DBP) using single readings taken at home or at the clinic. This study evaluated the fluctuations of SBP and DBP in continuous recordings of the arterial pulse waveform over short periods of time, and compared them to the maximum error allowed for a BP measurement device according to current standards. The analysis indicates that the natural variability of BP in healthy subjects results in a substantial number of individual beats in a short interval that exceed ±5 mmHg relative to the mean value over an interval (around one out of six readings). This is in the same range as we previously found in an analysis of a database of calibrated continuous photoplethysmographic pulse waveforms in healthy subjects (29.1% for SBP and 13.5% for DBP) and in a database of calibrated intra-arterial pulse waveforms in ICU patients (33.0% for SBP peaks and 14.9% for DBP) (Soueidan et al 2010b). Since the AAMI/ANSI-SP10 standard limits allowable measurement error to ± 5 mmHg, the results show that physiological variability likely contributes significantly to BP estimation uncertainty. In automated BP measurement devices, the situation is exasperated by the inevitable presence of uncertainty due to system errors.
This study addresses this problem with a new approach to provide more representative measures of SBP and DBP over a routine measurement interval, using simultaneous recordings of oscillometric and continuous arterial pulse waveforms. In a typical application, the proposed approach would provide clinicians and home users a concise output of the mean ± SD for each of SBP and DBP that substitute for the conventional values that are reported by automated BP measurement devices. When more details are desired, the approach is capable of providing a report with three measures to better characterize the BP: (1) the mean SBP or DBP over the measurement interval along with the confidence interval for the mean, (2) the standard deviation of the SBP or DBP over the measurement interval and (3) an indicator as to whether or not the oscillometric estimate is an outlier. The first measure (the SBP and DBP interval mean) is probably a better representation of a person's BP over the measurement interval than the SBP and DBP obtained at two random instants of time, and is likely stable over longer periods as has been established in a previous analysis (Soueidan et al 2010a). One commercial automated BP measurement device, BpTRU (Coquitlam, BC, Canada), has attempted to address the problem of representative values by averaging a minimum of five SBP and DBP readings taken over intervals of 1 or 2 min, and has been recommended to effectively diagnose and monitor hypertension (Beckett and Godwin 2005). The second measure (the interval standard deviation) characterizes the variability of SBP and DBP over the measurement interval. The third measure could be useful in providing an alert to the user or to a supervising clinician. A further analysis of the recorded signals may allow the determination if an outlier was due to a signal artifact, and so recommend repeating the measurement, or caused by an unusual physiological state.
The proposed approach was tested using a system equipped with two cuffs, each placed on one arm, and simultaneously inflated; the first cuff's pressure is kept constant, while the other's deflates at a constant rate. Two cuffs are not absolutely necessary for this method, as the continuous pulse waveform may be obtained using other non-invasive sensors. Although the testing involved a comparison between two laboratory systems, it nonetheless provides partial validation of the proposed approach since the oscillometric method underwent independent verification. Full validation of the proposed approach requires a study with a larger set of subjects (both healthy and hypertensive) in which the comparison is made with readings obtained by trained clinicians. The absolute accuracy of the proposed approach depends on the quality of the oscillometric estimate since this is used to calibrate the continuous pulse waveform. However, optimizing the oscillometric technique is outside the scope of this paper, and is the subject of on-going investigation by several groups (e.g. Baker et al 1997, Moraes et al 1999, Lee et al 2002, Amoore 2006).
In illustrative cases where the conventional oscillometric measures poorly represent the person's SBP and DBP over the measurement interval, the proposed approach clearly showed that it could usefully augment these measures. The incorporation of this approach therefore could improve the capabilities of existing oscillometric devices and so help address the unreliability and inconsistency of BP measurements in current practice.
Acknowledgment
This work was supported by Ontario Centres of Excellence and Biosign Technologies Inc.
Appendix
Appendix.
Table A1. Data collected from case 1.
| Oscillometric measurement | OMWDBP | 76.54 mmHg |
|---|---|---|
| Histogram of the DBP values over the 90 s of the recording, with the oscillometric reading identified by a star |  |
|
| Proposed method | INT_MEANDBP | 87.3 mmHg |
| INT_STDDBP (SD) | 7.79 mmHg | |
| Outlier | No | |
| Observations | Absolute difference (OMWDBP−INT_MEANDBP) = 10.76 mmHg OMWDBP is located within the (2×SD) margin from the INT_MEANDBP | |
| Interpretation | By visual inspection of the pulse waveform, the beat at which the oscillometric DBP was estimated does not appear artifactual. Although it might be misrepresentative of the average DBP over time, it accurately reflects the DBP at that instant in time and is located at a point of high physiological variability |
Table A2. Data collected from case 2.
| Oscillometric measurement | OMWDBP | 76.0 mmHg |
|---|---|---|
| Histogram of the DBP values over the 90 s of the recording, with the oscillometric reading identified by a star |  |
|
| Proposed method | INT_MEANDBP | 60.18 mmHg |
| INT_STDDBP (SD) | 7.69 mmHg | |
| Outlier | Yes | |
| Observations | Absolute difference (OMWDBP−INT_MEANDBP) = 15.82 mmHg OMWDBP is located beyond the (2× SD) margin from the INT_MEANDBP | |
| Interpretation | According to the chosen criterion, the oscillometric value would be considered to be an outlier. By visual inspection of the pulse waveform, the beat at which the oscillometric DBP was estimated does not seem to be artifactual but related to the natural variation of the BP signal. | |