Abstract
Very high frame rate ultrasound imaging has recently allowed for the extension of the applications of echography to new fields of study such as the functional imaging of the brain, cardiac electrophysiology, and the quantitative imaging of the intrinsic mechanical properties of tumors, to name a few, non-invasively and in real time. In this study, we present the first implementation of Ultrafast Ultrasound Imaging in 3D based on the use of either diverging or plane waves emanating from a sparse virtual array located behind the probe. It achieves high contrast and resolution while maintaining imaging rates of thousands of volumes per second. A customized portable ultrasound system was developed to sample 1024 independent channels and to drive a 32 × 32 matrix-array probe. Its ability to track in 3D transient phenomena occurring in the millisecond range within a single ultrafast acquisition was demonstrated for 3D Shear-Wave Imaging, 3D Ultrafast Doppler Imaging, and, finally, 3D Ultrafast combined Tissue and Flow Doppler Imaging. The propagation of shear waves was tracked in a phantom and used to characterize its stiffness. 3D Ultrafast Doppler was used to obtain 3D maps of Pulsed Doppler, Color Doppler, and Power Doppler quantities in a single acquisition and revealed, at thousands of volumes per second, the complex 3D flow patterns occurring in the ventricles of the human heart during an entire cardiac cycle, as well as the 3D in vivo interaction of blood flow and wall motion during the pulse wave in the carotid at the bifurcation. This study demonstrates the potential of 3D Ultrafast Ultrasound Imaging for the 3D mapping of stiffness, tissue motion, and flow in humans in vivo and promises new clinical applications of ultrasound with reduced intra—and inter-observer variability.
Export citation and abstract BibTeX RIS

Content from this work may be used under the terms of the Creative Commons Attribution 3.0 licence. Any further distribution of this work must maintain attribution to the author(s) and the title of the work, journal citation and DOI.
Over the last few years, 2D ultrasound imaging has undergone important technical improvements with the advent of software-based systems that enable the implementation of ultra-high frame rate imaging techniques: up to 20 000 frames s−1 are achieved, as opposed to the 50–200 frames s−1 used in traditional clinical systems. When such high frame rates are achieved in a large field of view, e.g. by using either plane wave ultrasound transmissions (Sandrin et al 1999, Tanter et al 2002), diverging wave transmissions (Couade et al 2009, Honjo et al 2010, Provost et al 2011b, Papadacci et al 2014a) or gating techniques (Pernot et al 2007, Wang et al 2008, Provost et al 2010), they allow for the study of rapid phenomena, such as the propagation of artificially-induced shear waves (Sandrin et al 2003, Bercoff et al 2004) and natural waves in tissues, e.g. the electromechanical wave in the heart (Provost et al 2011a) and the pulse wave in the blood vessels (Fujikura et al 2007, Couade et al 2010, Konofagou et al 2011). For this reason, it corresponds to one of the three categories of wave interactions in the field of multi-wave imaging (Fink and Tanter 2010). Moreover, such high frame rates improve temporal resolution, which in turn provides high-quality tissue motion mapping and blood flow mapping. For example, estimating the heart tissue motion above 500 frames s−1 results in a five-fold improvement of the elastographic signal-to-noise ratio (Provost et al 2012), while the increase in field-of-view and sensitivity of Ultrafast Doppler Imaging provides full-view cardiac blood flow maps and images of blood vessels with unprecedented resolution (Mace et al 2011, Demené et al 2014). These new techniques have bred entirely new fields of clinical applications for ultrasound imaging (Tanter and Fink 2014), such as the quantitative characterization of tumors (Tanter et al 2008), functional imaging of the brain (Macé et al 2011, Osmanski et al 2014), non-invasive imaging of cardiac electrophysiology (Provost et al 2013), the study of the arterial stiffness in hypertension (Vappou et al 2010), and high resolution vector flow imaging (Udesen et al 2008, Dort et al 2012, Ekroll et al 2013, Yiu et al 2014), to name a few.
Applying these techniques in 3D would significantly broaden their scope of application. For example, both shear and natural wave propagation occur in 3D but their quantitative assessment can only be done in 2D at the cost of simplifying assumptions. This aspect is crucially important when attempting to identify a pacing site in the heart for the treatment of arrhythmias (Provost et al 2013) or to detect the presence of mechanical anisotropy (Lee et al 2012). Moreover, generalizing Ultrafast Doppler Imaging to 3D would allow for new fields of study to emerge such as, e.g. the quantitative, fully non-invasive angiography of complex networks of blood vessels and the imaging of the cardiac fiber orientation (Papadacci et al 2014b). Unfortunately, existing commercial 3D ultrasound systems typically rely on hardware-based focused ultrasound beams and thus limited to a few tens of volumes per second. Although many approaches have been proposed in the literature to perform high volume rate volumetric ultrasound imaging (Perrin et al 2012, Denarie et al 2013, Skaug et al 2013), none, to our knowledge, provides sufficiently high volume rates to perform motion and blood flow measurement in an entire volume.
The concept of 3D ultrafast imaging at thousands of volumes per second relies on the transmission of a small number of ultrasound defocussed waves that insonify the entire volume of interest. Dynamic focusing is performed in receive whereas, in transmit, the coherent synthetic summation of the ultrasonic volume acquired for each transmission allows for the restoration of a dynamic focus without compromising the ultrafast volume rate. Montaldo et al applied this concept in 2D with plane wave transmissions, which resulted in coherent plane wave compounding (Montaldo et al 2009) and can be used for the simultaneous mapping of both flow and tissue velocities (Ekroll et al 2013) Recently, in the framework of ultrafast imaging of the human heart, we demonstrated the feasibility of compounding diverging waves using a sparse virtual array located behind the probe to achieve high frame rates and large signal-to-noise ratios in 2D in vivo at a limited cost in terms of resolution and contrast when compared to standard, low-frame-rate, focused imaging (Papadacci et al 2014a). Building on previous theoretical studies of sparse virtual arrays (Lockwood et al 1998, Hazard and Lockwood 1999, Nikolov 2001, Nikolov et al 2010), we report herein on the development of 3D Ultrafast Ultrasound Imaging based on the emission of diverging or plane waves emanating from virtual sources located behind a 2D-array ultrasound probe. By coherently compounding multiple emissions and by sampling the data of 1024 piezoelectric elements, we demonstrate that it is possible to perform 3D ultrasound imaging at thousands of volumes per second with large contrast and high resolution, in humans in vivo.
In this work, we introduce 3D Ultrafast Ultrasound Imaging and showcase potential clinical applications for cardiovascular imaging. More specifically, we describe the system architecture, validate the increase in contrast and resolution associated with coherently compounded emissions, and show the feasibility of motion estimation for shear-wave imaging in phantoms, of blood flow mapping in a full 3D field of view of the human heart, and of the simultaneous 3D mapping of both tissue and blood flow in the carotid artery near the bifurcation during the pulse wave propagation in vivo in humans.
1. Methods
1.1. System infrastructure
A customized, programmable, 1024-channel ultrasound system was designed to drive a 32-by-35 matrix array centered at 3 MHz with a 50% bandwidth at −3 dB and a 0.3 mm pitch (Vermon, Tours, France). The 9th, 17th and 25th lines were not connected, resulting in a total number of active elements equal to 1024. The 1024 independent channels could be used simultaneously in transmission, whereas receive channels were multiplexed to 1 of 2 transducer elements. Therefore, each emission was repeated twice, with the first half of the elements receiving during the first emission, and the second half of the elements receiving during the second emission.
All of the data processing, such as delay-and-sum volume beamforming and flow and motion mapping were performed on graphic processing units (K6000, Nvidia, Santa Clara, CA) in a Matlab environment (2013b, Mathworks, Cambridge, MA). Real-time bi-plane beamforming was also implemented for positioning, while volume beamforming was performed in postprocessing at a rate of, typically, a few volumes per second; the reconstruction rate decreased with the imaging depth, the number of compounded emissions, and the reconstruction sampling rate. 3D rendering was performed using Amira software (Visualization Sciences Group, Burlington, MA).
1.2. Image formation
A single framework consisting of virtual sources positioned behind the probe was used for compounding emissions (figure 1). More specifically, synthetic beamforming was performed using virtual sources forming a virtual array located behind the probe (figure 1(a)). For each source, a physical subaperture and a set of delays were computed (figure 1(b)). Emissions from individual sources were performed sequentially, and the radio-frequency data was recorded for each element of the entire physical probe. Volumes were beamformed using delay-and-sum algorithms for each virtual source and subsequently coherently compounded to form a final, high quality volume. Virtual arrays can be tailored to adjust resolution, contrast, signal-to-noise ratio, volume rate, and the field of view in a quasi-continuous fashion, therefore allowing for the selection of the optimal imaging sequence for a specific application (Lockwood et al 1998, Nikolov 2001, Montaldo et al 2009, Nikolov et al 2010, Papadacci et al 2014a).
Figure 1. 3D ultrafast ultrasound imaging framework. (a) Acquisitions are defined by a virtual array located behind the probe, which is then used to synthetically form an entire imaging volume. (b) For each individual source, delays are computed and a sub-aperture is defined. (c) When virtual sources are located near the physical probe, the sub-aperture used is smaller and the curvature of the emitted waveform is increased, which results in the insonification of a large field-of-view at the cost of a lower propagated energy. (d) When sources are located far behind the probe, larger sub apertures result in larger emitted energy, at the cost of a smaller field of view. In the extreme case of sources located at infinity behind the probe, tilted plane waves are obtained.
Download figure:
Standard image High-resolution imageIndeed, a number of trade-offs between contrast, resolution, volume rate, and field of view exist. For example, as the number of sources is increased, the contrast and resolution improve but the volume rate decreases, and as the distance of the virtual array decreases, the field of view increases but the contrast decreases. More specifically, positioning virtual sources onto the probe itself is equivalent to standard synthetic beamforming, with a high resolution and large field of view, but resulting in a poor volume rate and signal-to-noise ratio at larger depths. As the virtual array is moved behind the probe (figure 1(c)), additional physical elements can be recruited to contribute to one emission (i.e. the subaperture) and therefore increased energy is propagated into the tissue and larger signal-to-noise ratios are obtained (Lockwood et al 1998). The volume rate can also be adjusted by either increasing the pitch or decreasing the aperture of the virtual array up to the extreme case of using a single source (Provost et al 2011b), which is useful for applications requiring very high volume rates such as Ultrafast Doppler Imaging or Shear-Wave Imaging. Placing sources farther behind the probe leads to larger emission subapertures and a smaller field of view. Indeed, a virtual array at infinity (or very far, e.g. at 60 000 mm in this study) results in the emission of plane waves (figure 1(d)) with an imaging field of view corresponding to the 2D aperture of the physical probe.
Blood flow and motion estimation were performed by generalizing standard methods reported in previous studies. Namely, the Kasai algorithm (Kasai et al 1985) was used to estimate motion in phantoms and in tissues with a half-wavelength spatial sampling. Blood flow was estimated by first applying a high-pass filter to the baseband data and then, for each individual voxel; Power Doppler was obtained by integrating the power-spectral density; Pulsed Doppler was obtained by computing the short-time Fourier transform; and Color Doppler maps were obtained by estimating the first moment of the voxel-specific Pulsed-Doppler spectrogram (Osmanski et al 2014).
1.3. Experimental setup
Improvement in resolution was quantified as a function of the number of elements in the virtual array using a customized resolution phantom consisting of 1 mm metallic beads embedded in gelatin. This phantom contained a single layer containing 25 beads and was imaged at 5 different depths to generate a synthetic resolution phantom. Resolution was quantified by measuring the width at −3 dB of the main lobes for each bead. Contrast was quantified in a heart-mimicking phantom (067, CIRS, VA) by calculating the tissue-to-cavity B-mode amplitude ratio in at least 100 and at most 200 voxels at a given depth as a function of the number of sources, as well as in the common carotid of a healthy volunteer near the bifurcation. Shear-Wave Imaging was performed using two probes: the 2D matrix array was used to track the propagation of the shear wave in a 1.92 kPa phantom (acrylamide/bisacrylamide: 5%/0.05% w/w), whereas a standard 6 MHz, 1D linear array (L10-2, Supersonic Imaging, Aix-en-Provence, France), located approximately 2 cm away from the 2D array, generated three 100 µs radiation force 'pushes' approximately 2 cm away from the center of the 2D matrix array. The three push focal zones generated a Mach cone and thus an approximately conical shear wave. Note that the system could be used with the matrix array as a single probe to generate radiation force and to perform ultrafast imaging, but the experiment was not conducted in this study in order to avoid potentially damaging our customized probe. 3D Ultrafast Doppler Imaging was demonstrated by imaging the heart of a normal subject, and the feasibility of simultaneous 3D Ultrafast Doppler Imaging and 3D Tissue Doppler Imaging was shown through the observation of the propagation of the pulse wave in the carotid artery undergoing pulsatile flow.
2. Results
2.1. Resolution and contrast
Figure 2(a) shows the resolution phantom imaged using 1 and 81 virtual sources, respectively, at a 6 cm depth. One can observe an improvement in lateral resolution as the number of sources increased. Interestingly, however, as 3D focusing was performed at every voxel in receive, the resolution remained high, even when using a single emission.
Figure 2. Resolution and contrast. (a) An improvement in resolution is obtained when a larger virtual array is used. Indeed, as the number of virtual sources increases, the focal spot narrows and converges toward the optimal case of a focused emission in transmit and receive. Note that transmit–receive dynamic focusing does not lead to a large improvement of the resolution compared to receive only focusing. The improvement in terms of contrast is more important; even a small number of emissions can significantly increase the contrast both in phantoms (b) and in the carotid of a human subject in vivo (c). (b) Images of the heart-mimicking phantom in a view approximately aligned with a standard short-axis view (top) and a parasternal long-axis view (bottom). (c) Images of the carotid in cross-sectional and longitudinal views (top and bottom, respectively).
Download figure:
Standard image High-resolution imageIn terms of contrast, however, the situation was different: figure 2(b) (supplementary video 1 (stacks.iop.org/PMB/59/00L1/mmedia)) shows the improvement in contrast between the cavity and the tissue in a heart-mimicking phantom for varying depths as the number of coherently-compounded sources increased. The virtual array used had a pitch of 0.53 mm and a subaperture of 16 × 16 physical elements, and the imaging depth was 10 cm. Sources were added from the center as shown in figure 2. We can observe, as was the case in 2D (Papadacci et al 2014a), a rapid increase in contrast with the number of sources. Indeed, the first 10 dB increase in contrast could be obtained using 5 sources instead of one. To obtain a 20 dB increase, 9 sources had to be added, for a total of 16. A plateau was reached near the 30 dB mark, when 36 or more sources were used.
Similar results were obtained in vivo. Figure 2(c) shows the contrast improvement associated with the use of multiple virtual sources in the carotid of a normal subject in vivo. The 9 × 9 virtual array used was positioned at infinity behind the probe to generate plane waves angulated from −8 to 8 degrees with an imaging depth of 4 cm. A similar behavior was observed: a rapid increase in contrast occurred for the first few sources added before reaching a plateau. Notably, the plateau obtained corresponded to a smaller increase in contrast when compared against the phantom experiment of figure 2(a) and occurred at approximately 16 sources. This was, however, expected, as the motion of the tissue and blood, along with the hand motion of the sonographer, reduced the contrast enhancing properties of coherent compounding, especially when using a large virtual array requiring long acquisition times (8.4 ms for 81 sources with a 4 cm depth, i.e. 118 volumes s−1).
2.2. 3D Shear-Wave Imaging
3D Shear-Wave Imaging was performed using one virtual source located 2 cm behind the probe and a subaperture corresponding to the entire physical aperture at a rate of 3000 volumes s−1 with an imaging depth of 4 cm. Figure 3 (supplementary video 2 (stacks.iop.org/PMB/59/00L1/mmedia)) shows the propagation of the shear wave over a 3 cm distance from three different angles, i.e. from an approximately isometric view (figure 3(a)), from the top (figure 3(b)), and from the side (figure 3(c)). Its velocity was found to be approximately 0.8 m s−1, in accordance with the stiffness of the phantom used (Young's Modulus equal to 1.92 kPa).
Figure 3. Motion estimation for 3D shear-wave imaging. Propagation of a shear-wave generated using radiation force from an (a) approximately isometric view, from (b) a top view and (c) a side view. The velocity of the wave was found to be approximately 0.8 m s−1 and corresponds to the stiffness of the phantom used (1.92 kPa).
Download figure:
Standard image High-resolution image2.3. 3D Ultrafast Doppler imaging
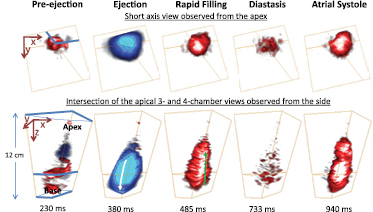
Blood flow estimation was performed in the apical view of the heart of a healthy volunteer at 2325 volumes s−1 and using a one-source acquisition with an imaging depth of 12 cm. A single ultrafast acquisition allowed the computation, in post-processing, of Color Doppler for each voxel of the volume. Color Doppler maps in which the Power Doppler data was used as a mask to perform the automatic 3D segmentation of the ventricles are shown in figure 4 (supplementary video 3 (stacks.iop.org/PMB/59/00L1/mmedia)). The Color Doppler ciné-loops in multiple complementary views and describing the different phases of the cardiac cycle in the left ventricle are shown: pre-ejection, ejection, rapid filling, diastasis, and atrial systole.
Figure 4. 3D Ultrafast Doppler Imaging in the heart. Blood flow in the left ventricle of a healthy volunteer during an entire cardiac cycle. After segmentation using the Power Doppler data, different well-known phases can be identified in the Color Flow Doppler ciné-loops, such as ejection and rapid filling.
Download figure:
Standard image High-resolution imageFinally, figure 5 (supplementary video 4 (stacks.iop.org/PMB/59/00L1/mmedia)) demonstrates how the high-quality acquisition using 81 sources can be used to display 1) the anatomy using a compounded B-mode, and combined to a one-source acquisition to quantify 2) Blood flow using Ultrafast Doppler Imaging and 3) motion of the carotid walls using Tissue Doppler. The Color Doppler maps were segmented using the Power Doppler data and overlaid onto the high-quality B-mode shown in figure 2(c) and acquired immediately after the 1 s one-source acquisition sequence at 3000 volumes s−1. The Tissue Doppler was overlaid onto the B-mode images and segmented by applying a dilation operation onto the Power Doppler mask. The bifurcation of the carotid could be identified and fully characterized as it was visible in both the high-quality B-mode and the Ultrafast Doppler Imaging ciné-loop. For instance, one can observe the Power Doppler Spectrum in any voxel, including at the entrance and exits of the bifurcation (figure 5). Figure 5 also shows the propagation of the pulse wave in the carotid wall (Couade et al 2010, Luo et al 2012); which is a flow velocity, pressure, and diameter waves generated at the ejection phase of the left ventricle (Nichols et al 2011).
Figure 5. 3D Ultrafast Doppler Imaging of the carotid bifurcation. Blood flow and tissue motion in the bifurcation of the carotid artery of a healthy volunteer overlaid onto a high quality B-mode volume during an entire cardiac cycle, along with quantitative blood flow shown for three regions at the entrance and exit of the bifurcation. The top view, which was cropped to the center of the carotid artery, can be used to clearly identify the location of the bifurcation.
Download figure:
Standard image High-resolution image3. Discussion
In this study, we have demonstrated the feasibility of 3D Ultrafast Ultrasound Imaging in humans in vivo. More specifically, we have shown that by using a virtual array located behind the probe, it is possible to achieve high contrast and good resolution with a small number of coherently compounded emissions, hence allowing for the imaging of thousands of volumes per second. Such high volume rates allow, in turn, for the accurate mapping in entire 3D volumes of Color Doppler, Power Doppler, Pulsed Doppler, and Tissue Doppler of each individual voxel. By implementing each algorithm on GPUs, it was shown possible to obtain these quantities in real-time or in a few seconds following acquisition depending on the required imaging depth and spatial sampling.
Figure 2 (supplementary video 1 (stacks.iop.org/PMB/59/00L1/mmedia)) demonstrated that coherent compounding can be used to achieve an optimal, application-dependent trade-off between contrast, resolution, and volume rate. Figure 3 (supplementary video 2 (stacks.iop.org/PMB/59/00L1/mmedia)) demonstrated the feasibility of both 3D Tissue Doppler and Shear-Wave Imaging for the mechanical characterization of tissues in 3D. Figure 4 (supplementary video 3 (stacks.iop.org/PMB/59/00L1/mmedia)) demonstrated the feasibility of Ultrafast Doppler Imaging can be performed in the challenging clinical setting of cardiac imaging in which we were able to fully characterize all the phases of the cardiac cycle. Finally, figure 5 (supplementary video 4 (stacks.iop.org/PMB/59/00L1/mmedia)) shows that 3D Ultrafast Doppler Imaging and 3D Tissue Doppler Imaging can be performed in the carotid in a single acquisition and overlaid onto a high-quality B-mode obtained at approximately 100 volumes s−1, which is more than sufficient for anatomical imaging.
3D Ultrafast Ultrasound Imaging could potentially revolutionize current clinical practices. Indeed, we have shown that by using 3D Ultrafast Ultrasound Imaging, blood flow can be visualized and quantified, e.g. in the totality of the carotid bifurcation, in order to identify the presence of abnormalities. Perhaps more importantly, the techniques detailed herein can be applied, theoretically, to any other organ. In the heart, a single 3D Ultrafast Ultrasound Imaging acquisition could provide 1) the 3D anatomy of all four cardiac chambers to measure standard quantities, such as the wall motion in all wall segments and the ejection fraction; 2) the quantitative blood flow, i.e. both pulsed and color Doppler, in each individual voxel of the volume to assess, e.g. all four valves' functions simultaneously and their relationships in the presence of obstacles or shunts in congenital cardiomyopathy; and 3) the cardiac displacement and strains in the entire heart both in their clinical form, e.g. peak systolic strains in all segments, or in novel versions requiring high frame rates, which can be used, e.g. to map the electromechanical activation sequence of the heart (Provost et al 2011a) or to locate ischemic regions (Lee et al 2011). Additionally, 3D Ultrafast Ultrasound Imaging could potentially complement or enhance existing techniques to image blood flow in 3D, such as magnetic resonance phase contrast velocimetry (Caroff et al 2012) or echocardiographic particle imaging velocimetry (Sengupta et al 2012), since it is portable and does not require ECG-gating or the injection of contrast agents. Additionally, in the presence of such contrast agents, since 3D Ultrafast Ultrasound Imaging is based on diverging emissions, it could further improve image quality both in terms of resolution (Desailly et al 2013) and contrast (Couture et al 2009, 2012).
Limitations to the technique include the reduced energy transmitted to the tissues, especially when a large field of view is needed, as it requires the use of spherical waves emerging from virtual sources located close to the probe. Indeed, the ultrasound pulse energy decreases as the square of the depth, without taking into account attenuation. This limitation can, however, be overcome by using the coherent compounding of multiple emissions, coded excitations, pre-amplified probes, or the development of higher-powered pulsers. Indeed, using compounded diverging waves allows for the safe propagation of large cumulative energy while ensuring limited tissue heating and small instantaneous local pressure, both of which are at the source of known potential adverse bioeffects. Moreover, the results of the resolution experiment of figure 2(a) are to be considered only qualitatively, as the metallic beads used were not sufficiently small against the focal zone size to provide quantitative resolution results; a complete quantitative resolution study is the object of on-going work.
Another important feature of 3D Ultrafast Imaging is the simultaneous acquisition of all radiofrequency element data within the observation volume. Such simultaneous and large field of view acquisitions can be used to improve image quality in post-processing, e.g. by allowing for the implementation of aberration correction techniques, which are currently known to be of limited interest in 2D as they do not account for out-of-plane aberrations. Moreover, motion compensation algorithms, for example in cardiac applications, as recently demonstrated in 2D (Denarie et al 2013), could be extended to 3D ultrafast acquisitions.
In conclusion, we have demonstrated the feasibility of 3D Ultrasound Ultrafast Imaging in humans in vivo is a novel approach for the simultaneous quantitative, functional, and anatomical imaging of tissues in 3D at very high volume rates. Such a technology allows for the mapping of blood flow and tissue motion in entire 3D fields of view and promises to enhance the current limitations of 2D echography in terms of inter—and intra-observer variability and to generate a host of novel 3D applications ranging from brain activation mapping and cardiac electrophysiology to ultrasound-based angiography and 3D Shear-Wave Imaging of tumors.
Acknowledgements
This work was supported by the European Research Council under the European Union's Seventh Framework Programme (FP/2007–2013) / ERC Grant Agreement n°311025 and by LABEX WIFI (Laboratory of Excellence ANR-10-LABX-24) within the French Program 'Investments for the Future' under reference ANR-10-IDEX-0001-02 PSL. J P is funded by a Marie Curie International Incoming Fellowship.